How panic attacks cause chest pain are due to several ways, including a few that involve the heart.
What’s quite fascinating is that the body mechanisms involved in a panic event may work in concert with each other rather than independent of each other.
How a Panic Attack Causes Chest Pain: Non-Heart Related Mechanisms
Musculoskeletal. During a panic attack a person may hyperventilate or breathe aggressively, causing pain in the chest via musculoskeletal strain. There may even be a spasm in the chest wall musculature.
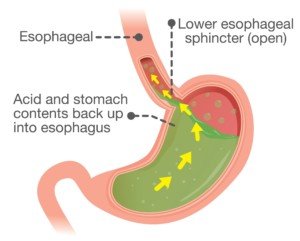
Esophageal. A sudden episode of anxiety or panic can trigger esophageal muscles to act up.
The esophagus is located “behind” the sternum, so naturally, if these muscles are in a state of dysmotility or dysfunction due to acute stress, you may feel chest pain.
Acid reflux can cause chest pain, and panic can cause a sudden reflux of the stomach’s acid upward into the esophagus.
Shutterstock/ solar22
“At the end of the esophagus and the beginning of the stomach, there is a sphincter (LES-lower esophageal sphincter),” explains Hugh Mai, MD, a gastroenterology and internal medicine specialist in Baltimore, MD.
“This is supposed to be a one-way valve that allows only food and fluid to come down from the esophagus into the stomach and not reflux — go back up into the esophagus,” continues Dr. Mai.
“A reflux-reflex response pertaining to GERD is the way that the body reacts when the brain is warned that acid is coming up from the stomach to the esophagus by the vagus nerve.
“The brain will try everything it can to prevent the acid from getting into the laryngeal structure (which is where the vocal folds are) and the lungs.
“To try to stop it, the brain sends a signal to the muscle in the esophagus to squeeze tightly, thus causing esophageal spasms and the so-called non-acid chest pain.”
How a Panic Attack Causes Chest Pain: Heart Related Mechanisms
A panic attack can cause chest pain due to involvement of the heart in a person with clean coronary arteries.
The physiological changes that are set off from a panic attack can cause a coronary artery to go into spasm. It doesn’t matter that the artery is free of plaque buildup. The spasm will hurt.
In fact, the spasm can actually temporarily impede blood flow in the heart, causing chest pain via this additional mechanism as well.
Remember though, this mechanical cause of obstructed blood flow does NOT indicate coronary artery disease (clogged arteries).
However, in those with pre-existing disease (clogged arteries), a panic attack can cause chest pain because it increases oxygen demand in the heart.
The arteries, constricted by plaque, cannot accommodate the increased blood flow that results from the increased oxygen demand. Chest pain (angina) results.
But wait – there’s yet another cardiac mechanism that potentially gets reeled in during a panic attack.
It’s called microvascular ischemia (aka small-vessel oxygen shortage). The heart contains very tiny arteries.
A panic attack will activate the sympathetic nervous system. This is the system that really kicks into gear when the body goes into “fight or flight” mode.
The sympathetic response increases tone (and thus resistance) in the microvascular coronary arteries. Mental stress or hyperventilation are believed to sometimes increase microvascular tone during a panic attack and hence cause chest pain in some individuals.
Duo of Cardiac and Non-Heart Causes of Chest Pain During Panic Episode
How a panic attack triggers chest pain can also be due to cardiac and non-cardiac mechanisms working together.
When one is faced with a threatening situation that triggers a panic attack, or when the panic episode arises spontaneously minus a situational trigger, the locus ceruleus might get stimulated.
The locus ceruleus is an area of the brain. Stimulation of this region increases anxiety and sympathetic tone – which can bring on increased heart rate, blood pressure and a shortage of oxygen flow in the heart: chest pain results.
Vicious cycle! The chest pain causes more panic, further stimulating the locus ceruleus.
You can see why, when a fit young person presents to an emergency room with chest pain, it can be vexing trying to figure out the cause when the tests look normal.
 Hugh Mai, MD, has 35+ years of experience and is well-versed in the endoscopic treatment of GERD. His areas of focus include interventional endoscopy, metabolic endoscopy and gut health.
Hugh Mai, MD, has 35+ years of experience and is well-versed in the endoscopic treatment of GERD. His areas of focus include interventional endoscopy, metabolic endoscopy and gut health.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.