Have you or someone you know been told they have “inflammatory lung disease”?
“Inflammatory lung diseases are clinically and histopathologically [under the microscope] a group of acute and chronic conditions,” begins Sashini Seeni, MD, a family medicine practitioner with DoctorOnCall, an online doctor and pharmacy.
“These disorders may affect the pulmonary vasculature, airspaces, pulmonary interstitium or a combination of these three anatomic compartments,” continues Dr. Seeni.
When my mother went to the ER the second time during a bout with pneumonia (she had vomited and complained of faintness and had clammy skin), a CT scan was ordered due to an elevated D-dimer.
The ER doctor said that the CAT scan showed that the pneumonia was gone (though my mother still had a bad cough).
The doctor then informed her, “The scan also shows that you have inflammatory lung disease, and this is not part of the pneumonia, which you no longer have.”
Interestingly, prior to the CT result, my mother had a chest X-ray that the doctor said still showed some pneumonia.
So I asked, “Then what was on the chest X-ray that you said a while ago showed some pneumonia?”
The doctor replied, “That’s scar tissue from the pneumonia. We know now from the CT scan that the pneumonia’s gone.
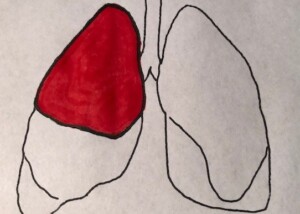
“Pneumonia tends to show on an image in a lobe of the lung, but the inflammatory lung disease shows as diffuse.
“I recommend a follow-up with your regular doctor or a pulmonologist to have your lung function checked.”
I asked the doctor for a more definitive explanation of this “inflammatory lung disease,” but he said it was difficult to be more descriptive at this point, and that’s why the follow-up was necessary.
I asked if this inflammatory lung disease could be caused by the pneumonia. He said no, pneumonia does not cause inflammatory lung disease.
I left the ER thinking that my mother possibly had some early stage lung disease! What was this inflammatory lung disease?
Inflammatory Lung Disease Could Be MANY Conditions
“Inflammatory lung disease can be divided into two subtypes which are infectious and non-infectious,” says Dr. Seeni.
“Non-infectious inflammatory lung diseases may be idiopathic [no known cause] or may represent a secondary reaction to autoimmune diseases, infections, environmental exposures or drugs.
“Meanwhile, some possible causes of infectious inflammatory lung diseases are tuberculosis, histoplasmosis and blastomycosis.”
COPD
“Chronic obstructive pulmonary disease (COPD), asthma and pulmonary fibrosis are the result of ongoing inflammatory processes,” says Dr. Seeni.
“COPD affects both the airways and lung tissue.
“This can manifest as a combination of emphysema and chronic bronchitis.
“COPD patients are most likely to have a smoking history.”
In addition, “Lung fibrosis is a chronic lung disease where the lung scars and thickens and that can affect oxygen exchange.
“The cause of lung fibrosis is unknown but for some reasons, it is believed to happen due to infection of the lung.”
Ground Glass What?
Next day I contacted my mother’s doctor’s office and spoke to the nurse.
I learned that the preliminary report of the CT scan, sent by the emergency room doctor, stated, “Granulatoma with change and ground glass opacities.”
It took me a while, but I finally recalled that several years ago, a “granuloma” was noted on a chest X-ray of my mother.
A granuloma is a dense collection of scar tissue that indicates previous infection and is harmless.
But what was this “ground glass opacities”?
Pneumonia can cause diffuse-pattern ground glass opacities (GGO) on a CT scan.
GGO can also result from an error in image interpretation, plus unreliable aspects of the imaging technology itself!
GGO can also appear as a result of normal breathing!
In short, GGO is a nonspecific radiologic finding that has a lengthy list of causes.
My mother had the follow-up, and the doctor apparently didn’t even mention the ground glass opacities, and was awaiting the more detailed report from the ER.
A phone appointment with my mother was made for two weeks later to discuss that more detailed report.
Two weeks later my mother’s doctor called and told her everything was normal, and that no further follow-ups were necessary.
The lesson here is: If you’re told you or a family member has “inflammatory lung disease” or “ground glass opacities” as revealed on a CT scan or X-ray, respectively, do not panic or lose sleep.
However, you should be quite discerning and inquisitive about this finding. Do not be reluctant to ask a lot of questions.

 DoctorOnCall
DoctorOnCall