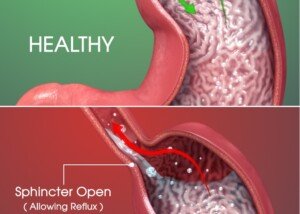
Ever wonder why ALL cases of Barrett’s esophagus aren’t just ablated away?
After all, wouldn’t this eliminate surveillance endoscopies and anxiety?
Furthermore, radiofrequency ablation is safe and highly effective.
With the endoscope, a tiny electrode delivers short bursts of a high-intensity heat form of energy to the precancerous tissue, destroying it.
So why not just perform this procedure on every case of Barrett’s esophagus to wipe out the worry and need for repeat upper endoscopies?
How Treatment Is Determined
“Treatment for Barrett’s is determined by findings from an endoscopic biopsy,” says Alex Little, MD, a thoracic surgeon with a special interest in esophageal and lung cancer.
“If cancer is found, that is staged and treated accordingly.
“If findings are normal except for the columnar epithelium [Barrett’s], the risks of cancer developing soon are minimal.
“The GERD is treated, and the endoscopy is repeated every three to five years (called a surveillance endoscopy) to monitor for possible development of early cancer or a premalignant condition called dysplasia.
“There are treatment options when dysplasia is found.
“If the dysplasia is termed ‘low grade’ (meaning the cells are only slightly abnormal), gastroenterologists usually follow the patient with GERD therapy and surveillance more frequently than for patients with no dysplasia.
“If the dysplasia is more advanced and called ‘high grade,’ the treatment plan most favored at present is as follows.
“An extensive search is performed for cancer that the biopsies may have missed; this includes CT scans and endoscopic ultrasound exam of the esophagus.
“In the past, regardless of whether cancer was found, an esophagectomy [removal of the esophagus] was performed because of the risk of current or future cancer.”
A new food pipe would be constructed with tissue from the stomach.
Dr. Little continues, “Now the recommendation is for an ablative procedure (with destruction of the abnormal epithelium with a laser) or an endoscopic removal of the abnormal epithelium.
“After both treatments the patient continues treatment for GERD, and surveillance endoscopy is performed.”
So even if you undergo ablation for a high grade of Barrett’s esophagus, you would still need to undergo repeated endoscopies.
 Alex Little, MD, trained in general and thoracic surgery at the Johns Hopkins University School of Medicine; has been active in national thoracic surgical societies as a speaker and participant, and served as president of the American College of Chest Physicians. He’s the author of “Cracking Chests: How Thoracic Surgery Got from Rocks to Sticks,” available on Amazon.
Alex Little, MD, trained in general and thoracic surgery at the Johns Hopkins University School of Medicine; has been active in national thoracic surgical societies as a speaker and participant, and served as president of the American College of Chest Physicians. He’s the author of “Cracking Chests: How Thoracic Surgery Got from Rocks to Sticks,” available on Amazon.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.