
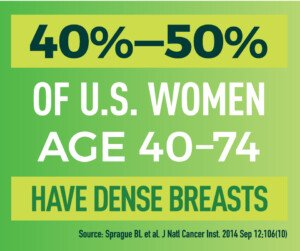
Very dense breasts are third in line as a major risk factor for cancer; so why won’t the medical establishment support elective removal like it does for BRCA mutations?
Only family history (first degree relative) and the BRCA mutations trump extremely dense breasts as the biggest non-changeable risk factor for breast cancer.
By law, insurance must pay for prophylactic removal of both breasts when a woman tests positive for BRCA1 and BRCA2.
A fair question is just how far behind that No. 3 spot, for extreme breast density, is behind the No. 2 spot of BRCA1 and BRCA1.
Keep in mind that the older a woman is, the more relevant age becomes as a risk factor.
- Is that No. 3 spot WAY behind the No. 2 spot?
- Or is the gap really small?
The answer is not known.
Nevertheless, women with extremely dense breasts (a “D” classification) have certainly wondered about elective removal — even if they were negative for BRCA mutations and did not have a first-degree relative with breast cancer.
What makes the issue of extremely dense breasts even more problematic is that they are more difficult to read on mammography.
Dense breast tissue appears as white. But so does a malignant tumor.
“It’s true that dense breasts are more difficult to be evaluated by mammogram, and thus, a cancer may be diagnosed later,” begins Dr. Kimberly Langdon, MD, OBGYN, medical advisor at Medzino Health, an online doctor and pharmacy site.
“But for now, there is no recommendation for prophylactic removal of them,” continues Dr. Langdon.
“There are better tests such as MRI that can be used to monitor dense breasts, though.
“Speak with a doctor who specializes in breast cancer to see what your options are.”
You may be wondering about getting tested for a BRCA mutation even if your mother, sister or daughter have never been diagnosed with breast cancer.
You might be told that unless a first-degree relative has had breast cancer, insurance will not cover the BRCA test — and in fact, that you don’t even qualify for the test.
This is what had happened to me — I had very dense breasts.
But I replied, “Just because one of my sisters or mother never had breast cancer doesn’t mean I can’t have a BRCA mutation, nor does it mean none of them do either.”
My risk assessment was 13% due to a cousin having had breast cancer.
It was left at that.
Some years later I received a letter from my sister, revealing that 13 months prior, she’d been diagnosed with breast cancer.
I immediately contacted my health care provider and inquired about the genetic testing. This lead to a lengthy risk assessment over the phone. My risk was now 21%.
Expecting to be told that the test would be set up for me, I was instead told that I qualified for either at least five years of taking a hormone drug, or a preventive bilateral mastectomy covered by insurance.
Well of course, I told her right then and there to get the ball rolling for the elective double mastectomy.
My sister had never been tested for a BRCA mutation. We’ll never know if she, or anyone else in my family, has it.
What I DO know is that her mammograms had been the 2D type — which is less sensitive to mass detection than the 3D type — called tomosynthesis — depicted below.
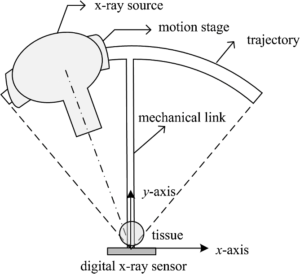
Three-dimensional mammography: tomosynthesis
The mammogram she’d had a year prior to the one that revealed the tumor had been negative.
It’s very fair and wise to wonder if, had that second-last mammogram been 3D, would it have caught the cancer at a much earlier stage?
After all, her diagnosis turned out to be stage 2B, which isn’t a very early catch. It had already infiltrated axillary lymph nodes.
The prognosis is considered good, in that the five-year survival rate is about 85%.
But for stage 1 it’s 98 to 99%.
Summary
• Extremely dense breasts are a risk factor for breast cancer, a non-modifiable feature that’s ranked behind immediate family history and BRCA mutations.
• How far behind is not known.
• You have a right to receive information about your breast density, which can only be determined by a mammogram. It cannot be determined by cup size, a doctor’s palpation or how the breasts appear in a mirror.
• Women with dense breasts should combine annual screening ultrasounds with their annual mammograms – which should be the 3D type (tomosynthesis) that’s more sensitive to showing suspicious masses.
 Dr. Langdon, who is now retired from clinical practice, has delivered over 2,000 babies. Besides obstetrics, she specialized in gynecologic situations such as menstrual disorders, vaginitis, menopause, contraception, pelvic pain and minimally-invasive surgeries.
Dr. Langdon, who is now retired from clinical practice, has delivered over 2,000 babies. Besides obstetrics, she specialized in gynecologic situations such as menstrual disorders, vaginitis, menopause, contraception, pelvic pain and minimally-invasive surgeries.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.









































