It would seem that most patients with advanced heart failure who are getting worse would be suitable candidates for a ventricular assist device.
There was the case of a woman, who appeared to be middle-aged, and was posting her experiences with terminal congestive heart failure on YouTube.
- She had been given 10 days to live, but a few months later was still alive—though in hospice status.
- She was confined to her bed while talking for her YouTube videos.
- She had supplemental oxygen.
- She was lucid and coherent.
- Yet she was dying.
There are many people in the same boat, from her age to very elderly, who are rapidly declining and are told it’s the end for them.
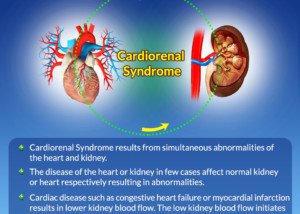
A ventricular assist device (VAD) would help the heart pump blood, increasing systemic circulation, thereby improving kidney and liver function and reducing strain on the heart.
But the ventricular assist device is not typically offered to severe heart failure patients, or those suffering from acute decompensated heart failure who are getting worse by the day.
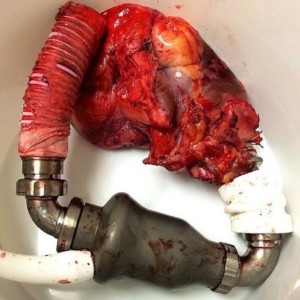
“VADs are typically used as a bridge to heart transplant for patients with end-stage heart failure – i.e., medications are not working and the only option is heart transplant or the patient will expire (over some reasonably short period of time),” says Mark Pool, MD, a board-certified cardiothoracic surgeon based in TX who’s been in private practice since 2011.
Ventricular Assist Devices in Patients Not Suitable for Heart Transplant
“VADs are also used as destination therapy, meaning that the ventricular assist device is not a bridge to something else (transplant) but the final and definitive therapy,” explains Dr. Pool.
“This might be for a patient considered too old for a transplant or for whom a transplant is contraindicated.”
One reason for contraindication of a heart transplant is poor kidney function.
The kidneys take the so-called big hit during an organ transplant.
Decently functioning kidneys can withstand this hit. Kidneys with enough of a pre-existing insufficiency can’t – and such a patient thus would not survive the surgery.
Another reason a heart failure patient is sometims not a candidate for heart transplant is advanced age and overall weakness, especially if there are comorbidities (e.g., blood pressure problems, coronary artery disease).
Dr. Pool continues, “Certainly, undergoing the operation [VAD placement] is a daunting task, and there again we see the difficult balance of figuring out who is right for one: profoundly sick patient who is weak and getting worse — hmmm, doesn’t sound like a good candidate for a major heart surgery.”
“But, sometimes, a ventricular assist device is the only therapy that will (likely) preserve the patient’s life.”
Surgery for a ventricular assist device requires cracking open the chest: full-fledged open heart surgery.
The irony is that the very patient who desperately needs the VAD may also be too weak to survive this operation!
Usually this would be a very elderly person with very poor cardiac and renal function.
In these cases, the medical team has no way out, and opts for letting nature run its brief-remaining course, as it would be medical malpractice to attempt this surgery on such a patient.
“VADs and transplants are usually performed at centers with large teams of heart failure specialists so that the decision-making for these very complex patients does not fall to only one physician, but the collective wisdom of the team can help make the proper choice,” says Dr. Pool.
Why Aren’t Ventricular Assist Devices Used More Often As Destination Therapy?
Dr. Pool explains, “VADs are not used more often for a variety of reasons such as – a patient too weak to survive the surgery, financial constraints (a hot-button reason, perhaps, but the reality is that VADs are extremely expensive, not just to put in, but the care for them afterwards is extremely expensive and they are not generally implanted for patients without insurance or other considerable financial resources), patient in a facility where VADs are not an option so it is never discussed as a possibility.”
What if there is no hope for the patient (not a transplant candidate), and the patient is covered by insurance?
If the patient is very sick with acute heart failure along with acute kidney failure, and to make matters worse, is very elderly and has comorbidities, the medical team most likely won’t even think about a ventricular assist device – especially if the facility doesn’t specialize in the treatment of acute heart failure and instead is a standard hospital setting.
Even in younger patients coming in with an acute process, the placement of a ventricular assist device comes with potential risks that, on an overall basis, outweigh the potential benefits.