
You’d be shocked to know just all the ways that sleep apnea can harm the heart.
If you’ve ever wondered why periods of stopped breathing can be so dangerous to the cardiovascular system even though the heart doesn’t actually stop beating, you’re about to find out.
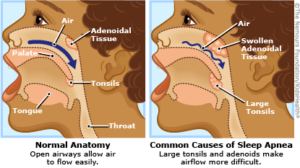
Sleep apnea is usually the obstructive type. This means that while you’re asleep, the structures and tissues of the upper airway collapse.
This may partially or completely obstruct the passage of inhaled air coming through.
If it’s a complete obstruction, the person will stop breathing.
However, the brain eventually senses a drop in oxygen levels, and rouses the sleeper — just enough to unrelax the airway tissues and allow for a deep breath.
Then the process starts all over again — all through the night.
Sleep apnea affects all ages.
What this all means is that the oxygen levels in the body are dropping (desaturation), then rising (re-saturation) with recovery breaths, then falling again, back and forth.
“Recurrent desaturation and re-saturation and recurrent arousals leads to fluctuations in pleural [surrounding the lungs] pressure and strains the heart, and can cause bradycardia and then tachycardia,” says Dr. Nancy Foldvary-Schaefer, DO, MS, and Director, Sleep Disorders Center, Cleveland Clinic.
- Bradycardia: abnormally slow heartbeat
- Tachycardia: abnormally fast heartbeat
”The heart should rest in sleep, but in the presence of significant OSA, the heart is actually working harder than it should be,” says Dr. Foldvary-Schaefer.
“Long-term, recurrent apneas associated with hypoxia [abnormally low oxygen] and arousal lead to a pro-inflammatory state that drives cardiovascular events, stroke and hypertension: systemic and pulmonary.”
A Closer Look at Untreated Sleep Apnea’s Danger to the Heart
The collapsed airway subjects the body to ongoing periods of:
• Hypoxia
• Abnormally low pressure within the chest/lung cavity
• Brain arousals
More specific harm then follows:
• Reduced contractile ability of the heart muscle
• Heart muscle wall stress
• Activation of the sympathetic nervous system—the “flight or fight” response
• Increase in blood pressure
• Increased heart rate
• Body-wide inflammation
• Platelet activation (aka thicker blood; higher blood clot risk)
• Impairment of the inner lining of blood vessels (endothelium)
Whew! That’s a lot! But that’s just the beginning.
For example, that impaired endothelial function can lead to increased stiffness of the arteries – which then can bring on high blood pressure throughout the day.
Now wait a minute here. If the sleep apnea ends when you awaken, why would you have high blood pressure throughout the DAY?
It all originates during sleep when you stop breathing. Remember, OSA drops the body’s oxygen level, arousing the brain — just enough to send signals through your nervous system to get you breathing again, but not enough to awaken you to full consciousness.
Obstructed airway. Habib M’henni, Wikimedia Commons
The signals instruct the blood vessels to increase the flow of oxygen to the heart and brain. However, this mechanism may carry over to after you’re awake.
The low oxygen levels (desaturation) during sleep trigger several mechanisms that persist during waking hours – ripples in the pond that continue to expand outward.
At the end of any given overnight apneic event, blood pressure may be as high as 240/130.
However, “One can have low blood pressure and still have OSA,” says Dr. Foldvary.
This is because, for reasons researchers don’t yet know, some patients — even those with severe OSA (as measured by the average number of sleep disordered events per hour) — don’t experience symptoms during wakefulness.
Untreated Sleep Apnea: Body Lying Still but Overworking
It’s one thing when your body works hard during conscious daytime exercise at the gym.
It’s a whole new, and brutal, animal when your body is overworked overnight due to stopped breathing and desaturation.
The overwork due to sleep apnea thickens the walls of the heart. That may sound like the heart gets stronger like a biceps muscle, but biceps muscle and heart muscle are not the same kind of muscle.
You do NOT want the walls of your heart to thicken. This enlargement makes the heart get less oxygen and work less effectively.
Furthermore, the overnight workload changes the structure of your heart.
It becomes stiffer because more (and undesirable) fibrous cells grow between the cardiac muscle cells.
You eventually resume breathing, so what’s the big deal?
Frequent bouts of hypoxia damage the blood vessels that supply oxygen to the heart.
Recurring hypoxia causes the release of substances that may cause constriction of blood vessels for hours.
Obstructive sleep apnea can lead to chronic heart failure via several routes:
• Activating the sympathetic nervous system, including during waking hours.
• Increasing left ventricular workload, including during wakefulness.
• Increasing right ventricular workload.
All of this can then lead to atrial fibrillation, a rhythm disorder. And guess what: another ripple, in that atrial fibrillation is a major risk factor for stroke and heart attack!
Are you now getting the impression that sleep apnea’s ripples in the pond are created by a boulder?
If someone tells you they think you have sleep apnea, but they’re not a doctor, don’t let that stop you from SEEING a sleep doctor.
• Don’t make excuses like “I’m old.”
• Regardless of cause of OSA (obesity, smoking, naturally narrow upper airway, excess throat tissue), the damage to the body is the same, and in most cases, the treatment is the same.
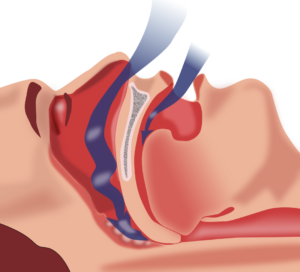
The gold standard of treatment is CPAP: continuous positive airway pressure — shown below.

CPAP machine. Shutterstock/Brian Chase
In some cases, OSA can be mitigated by a custom-made mandibular device to place inside the mouth overnight, fashioned by a sleep dentist.

 Certified by the American Board of Neurology and Psychiatry in Neurology, Clinical Neurophysiology and Sleep Medicine,
Certified by the American Board of Neurology and Psychiatry in Neurology, Clinical Neurophysiology and Sleep Medicine, 
































