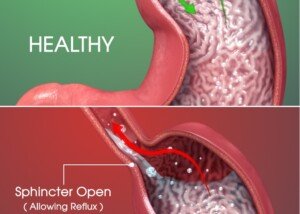
Reflux esophagitis is inflammation of the esophagus from prolonged contact with corrosive stomach acid. Does this always cause symptoms?
Acid to break down food should remain in the stomach. But in some people it refluxes up into the esophagus.
If this happens often enough, the inner wall of the “food pipe” will become inflamed, which over time, can lead to an ulcer. The ulcer may then bleed.
“People have variable pain thresholds, and the symptoms of reflux can be very different from the common description of intense heartburn,” says Joseph Weiss, MD, a board certified gastroenterologist and clinical professor of medicine at the Medical School, University of California, San Diego.
One would think that the severity of symptoms would correlate, in a predictable and linear fashion, to what an upper endoscopy shows.
But this isn’t the case. Up to half of patients with heartburn may have a normal-looking esophagus as revealed via upper endoscopy.
Oddly, people whose scope reveals esophageal damage may be symptom-free.
I went in for an upper endoscopy (EGD) because I was experiencing several symptoms (that were for the most part, relieved with Nexium).
One symptom was discomfort in a small area a few inches to the right of my breastbone (sternum) two seconds after swallowing food.
Another symptom was periodic burning in my throat. A third was occasional but very mild reflux of food.
The fourth was excessive burping. I suspected reflux esophagitis.
How could I NOT have inflammation if I was feeling discomfort two seconds after swallowing food?
By the time I had the EGD, I’d been on Nexium for many weeks, and for the most part, the symptoms had been calmed down.
My EGD was perfectly normal. My gastroenterologist said that there could’ve been past inflammation that was now gone.
What’s stranger is when there’s a visible injury via the EGD, but the patient is asymptomatic.
Severity of symptoms, or absence thereof, is a poor predictor of the extent of esophagitis.
Erosive esophagitis can actually be present in a person without symptoms, according to reports.
What may be troubling to someone is that erosion in their esophagus may be taking place without them knowing it due to lack of symptoms.
Chronic contact with stomach acid can lead to Barrett’s esophagus, a precancerous condition.
Up to one-fourth of patients with Barrett’s esophagus experience no symptoms.
The same studies show that only one-third of people with esophageal strictures (narrowing) have a history of GERD (gastroesophageal reflux disease, or chronic acid reflux).
Why don’t some people experience symptoms?
How could someone not “feel” that the inside of their food pipe is inflamed or wounded?
This may come down to individual perception that can translate to reduced sensitivity.
- Those with Barrett’s esophagus have a higher threshold of symptom perception when compared to healthy controls or those with GERD but no Barrett’s.
- People with severe reflux esophagitis, mainly those who have Barrett’s or an esophageal stricture, don’t necessarily have symptoms of acid reflux or GERD.
Furthermore, don’t let all those TV commercials trick you into thinking that reflux causes only heartburn. There can be many different symptoms.
“These ‘atypical’ GERD symptoms can include chest pain, difficulty swallowing from stricture, loss of tooth enamel, laryngitis, voice strain, asthma, cough, nausea, vomiting, aspiration pneumonia, etc.,” says Dr. Weiss.
 Dr. Weiss is the author of Got Guts! A Guide to Prevent and Beat Colon Cancer. He has also presented numerous presentations on various health topics.
Dr. Weiss is the author of Got Guts! A Guide to Prevent and Beat Colon Cancer. He has also presented numerous presentations on various health topics.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.