Here’s what it’s like to undergo a back to back or combined upper endoscopy with a colonoscopy, a step by step first-person account.
What you first must do is select a reliable person to drive you to the procedure, so you can then be driven back by that individual.
I underwent a combined upper endoscopy and colonoscopy.
I’m going to narrate exactly what happened and how everything felt, every step of the way.
First off, you need NOT have any anxiety just because you’re undergoing two back to back procedures.
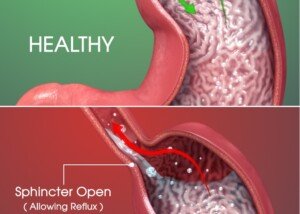
The reason I had a combined upper endoscopy and colonoscopy was because I was due for a screening colonoscopy, but I was also having issues with acid reflux, so I requested an upper endoscopy.
Getting both done at the same time is the way to go.
What It’s Like to Have a Combined Upper Endoscopy and Colonoscopy
I was told to remove my pants and underwear, but keep my shirt on, and lie on the bed in the exam room.
My vitals were taken. A nurse covered me with a warm blanket and then set up an IV port in my arm.
You should feel free to ask the nurse any questions, such as the names of the drugs you’ll be given for the procedures.
In my case it was Benadryl, Fentanyl and Versed.
For quite a while I was alone in the room, under the warm blanket; no drugs yet.
How long you’ll be waiting depends on whether the doctor is held up. In my case, much of the delay was due to COVID-19 protocols.
Finally, I was wheeled to the procedure room, where I met the gastroenterologist for the first time – having already had a phone consultation with her several weeks prior.
There were at least two other nurses present.
A nasal cannula for supplemental oxygen was placed. I asked why and was told that the Fentanyl suppresses breathing.
I was told to lie on my left side and that the upper endoscopy would be done first.
Anxiety over how the upper endoscopy will feel?

Upper endoscopy
As you probably already know, an upper endoscopy requires that the doctor insert a “tube down your throat,” down your esophagus and into your stomach and small intestine.
As I lie there, I wasn’t worried about how this would feel. I had a gut feeling (no pun intended) that the drugs would knock me out.
I was just hoping that my esophagus would be normal.
A nurse took my right arm, the one with the port. I asked her what drug she was putting in me, and she said Fentanyl.
Within seconds, I began feeling a heaviness descend upon me, as though Earth’s gravity was suddenly getting heavier. Simultaneously I began feeling dizzy.
While this was happening I was facing two other nurses, or possibly just one nurse and the doctor.
My exact words were, “Oooh, I can feel that.”
They smiled.
Realizing that I was still lucid, I repeated, “I can really feel that.” I wondered when I would start becoming loopy.
I asked for a pillow to be placed between my legs.
A nurse mentioned there were no pillows but that she could fold up a blanket and put it there.
I said something to the effect of “Yes, put a blanket there and fold it like a pillow.”
Something then made me close my eyes. I heard the doctor say something like, “I’m putting in the mouth clamp.”
Then I heard her telling either me or another nurse, as she stood right by the bed, that my esophagus was normal.
I opened my eyes. She and a nurse were right by the bed. I asked if my esophagus was normal, and she said yes.
I watched at least one person walk around the other side of the bed (facing my behind, as I continued lying on my left side).
Next thing I knew, I began feeling abdominal pain near the belly button.
It began creeping upward and getting worse. Eyes still closed, I moaned briefly and said, “It hurts.”
I remember thinking that I wanted to tell the doctor to “take it out” (meaning the scoping instrument), but I’m pretty sure I refrained from saying this.
I’m not sure, but I believe someone then said that they never gave me one of the drugs (either the Benadryl or Versed) because my heart rate had been too high (from anxiety), and that’s why I was feeling the pain.
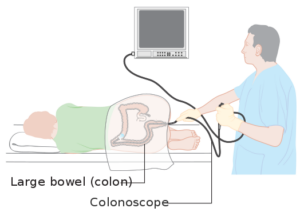
Colonoscopy. Cancer Research UK
It’s All Over
Next thing I knew, I heard the doctor, who was standing on my left but away from the bed, mention something about finding a polyp.
I opened my eyes and turned on my back, and the doctor walked to my right side.
I don’t remember if I asked if she found a polyp, or if she told me this first.
I rapidly became lucid and a brief discussion about the “small” polyp followed.
I was given paperwork detailing everything, including printed-out images of the interior of my esophagus, stomach and colon.
One of the images was of the polyp, which had been removed (ultimately it was diagnosed as a benign hyperplastic type. These common polyps are nothing to worry about).
I had no complications, no cramping, no nausea, but when I got home, still feeling a bit woozy, I took a nap for about an hour and 15 minutes.
Then I ordered two personal pan pizzas and brownies from Pizza Hut!
Ask Questions Beforehand
The more questions you get answered ahead of your combined upper endoscopy and colonoscopy, the more at ease you’ll feel once you’re in the initial exam room.
Don’t assume. Don’t guess. You have every right in the world to ask your doctor anything.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.