It’s just plain total anxiety when a skin sample is sent off for a biopsy, especially when you did not expect this to happen, and all you can think of is “What if it comes back as melanoma?”
If this occurs on a Friday, your entire weekend will probably be shot down with intense anxiety.
First off, most skin samples that are sent for biopsy do not come back as cancerous, especially when different kinds of samples are included in the analysis, vs. only those moles that a dermatologist thinks are suspicious.
A study (JAMA Dermatology, Piepkorn et al) involved an analysis of over 80,000 samples of skin tissue.
“There’s a wealth of information in electronic medical records that has been untapped for population-level studies like this,” explains one of the study authors in the paper.
“Text-analysis software is especially helpful to decipher pathologists’ reports, because they have a wide array of terms for the same type of lesion.”
Another name for a common skin mole is melanocytic lesion.
“Melano” refers to pigment-producing, and “cytic” refers to cell: pigment-producing cell.
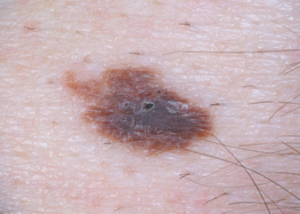
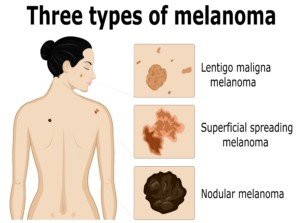
Melanoma can arise from a benign mole or from a non-melanocytic area of skin.
One-third of these cancers arise from pre-existing moles.
Study: Determining How Many of Over 80,000 Skin Samples Were Positive for Melanoma
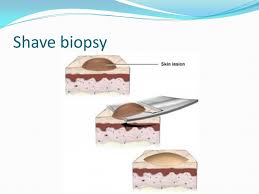
The biopsies of a variety of skin lesions (not just moles) spanned between January 2007 and December 2012, from over 47,000 patients in the Group Health Cooperative healthcare system (known now as Kaiser Permanente) in Washington.
Of the 80,000+ samples, 23 percent were identified as melanocytic lesions (moles).
However, the identification that a lesion was a mole did not always mean that the entire mole was benign. In some cases, there were cancerous portions.
• Class I: Entire mole was benign (83 percent)
• Class II: Moderately dysplastic (containing abnormal though not malignant cells) and other low-risk lesions (8.3 percent)
• Class III: Melanoma in-situ (confined to only the top layer of skin) and other higher-risk lesions (4.5 percent)
• Class IV/V: Invasive melanoma (4.1 percent)
The above bullet points refer strictly to the 23 percent of samples that were determined to be pigment-producing lesions – ranging of course from completely benign to being melanoma.
The remaining 77 percent of samples were not moles, or to put another way, were non-melanocytic.
These skin growths included those caused by sun damage, viruses or infections.
The growths that were caused by sun damage included basal cell carcinoma and squamous cell carcinoma.
These skin cancers are far less deadlier than melanoma.
Shutterstock/Scio21
In fact, basal cell carcinoma is extremely slow growing, extremely curable, and metastasis is exceptionally rare.
Anxiety Waiting for Biopsy Results
It can be reassuring to know the following:
A stage 0 melanoma has a 10 year survival rate of 99%.
The five year survival rate for stage 1 disease is around 95%.
When caught early, melanoma is highly curable … but …
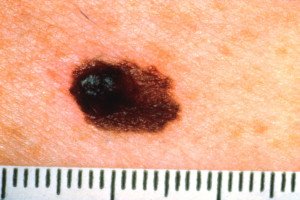
Invasive melanoma
… the prognosis is very poor when it’s caught in a later stage.
Taking precautions regarding sunlight exposure goes a very long way at preventing melanoma, says Alberto de la Fuente Garcia, MD, a board certified dermatologist at VIDA Wellness and Beauty with 15+ years of experience.

Melanoma
“Exposure to ultraviolet (UV) radiation from the sun and other sources can damage your skin cells, leading to premature aging and an increased risk of developing skin cancer,” says Dr. de la Fuente Garcia.
“A good way to protect yourself from UV radiation is to limit your exposure and use sun protection whenever you go outside.
“This means wearing a hat and clothing that covers your skin, avoiding direct sunlight during the peak hours of 10 am to 4 pm, and using sunscreen with SPF 30 or higher.
“Try to stay in the shade as much as possible, avoid tanning beds and sunlamps, and use window film or curtains to reduce the amount of UV radiation entering your home.”

 Dr. de la Fuente Garcia
Dr. de la Fuente Garcia