Do you keep reading that an acoustic neuroma “can be fatal”?
Is this scaring the daylights out of you, especially since your tinnitus has not yet been evaluated?
It’s true that an acoustic neuroma can lead to death. However, in this era of modern medicine, a lethal acoustic neuroma is more hypothetical than reality.
The key words are “left untreated.”
So you’re probably thinking, “Who doesn’t get their acoustic neuroma treated? The symptoms as the tumor grows eventually cannot be ignored.”
“And why do so many medical sites say that an acoustic neuroma can be fatal”?
An even more compelling question is: Can an acoustic neuroma kill a person before it starts causing symptoms?
Why an Acoustic Neuroma Can Be Fatal
“Prior to modern medical imaging, fatality from these tumors was not uncommon,” explains Brandon Isaacson, MD, F.A.C.S., Department of Otolaryngology – Head and Neck Surgery, UT Southwestern Medical Center, Dallas, TX.
“In this day and age it is quite rare [dying from an acoustic neuroma] except in patients with no access to medical care,” says Dr. Isaacson.
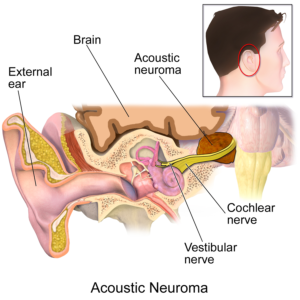
“Death from a large acoustic neuroma occurs secondary to obstructive hydrocephalus (spinal fluid has no way to exit the ventricular system within the brain). This causes the brain to protrude through the base of the skull.
“Other mechanisms for fatality include having a stroke or a heart attack during or after surgery (<1%), or developing a cancerous tumor after radiation (1:1000).”
The 1:1000 refers to malignant transformation, not mortality.
Medical sites need to be fair. This is why it’s proper for them to state that an acoustic neuroma CAN be fatal. This statement, as accurate as it is, cannot be used as a predictor for survival.
That’s because in a realistic setting, these tumors DO get treated. It’s very difficult, even for someone without medical insurance, to ignore the symptoms.
BruceBlaus
Symptoms
Progressive hearing loss
Tinnitus that can be quite troubling
Facial paralysis
Balance problems
Headaches that won’t go away.
Even a mentally ill shut-in with no family or friends will likely eventually seek out a doctor for these symptoms as they become unbearable.
Of course, someone who lives in a remote area of a developing country who develops these symptoms may never see a doctor – and hence, die from their acoustic neuroma.
Nevertheless, people in industrial nations have died as a result of their acoustic neuroma.
But this mortality is related to surgery. The larger the tumor the higher the mortality rate following surgery. Causes of death, due to surgical complications, may also be from:
• Softening of the outer side of the pons, a part of the brainstem involved in critical functions including breathing.
• Bleeding blood vessel in the pons.
• And as mentioned, malignant transformation of the tumor years after radiation surgery. Radiosurgery doesn’t remove the tumor; it either shrinks it or stops it from growing.
Malignant transformation of the residual mass is EXTREMELY rare – just a handful of cases reported in medical literature.
In summary, an acoustic neuroma will likely become fatal if left untreated.
It’s not realistic that it will grow larger than a ping pong ball without producing any symptoms.
When a treated acoustic neuroma leads to death, this is due to a rare complication of surgery.
Update: Study Examines Watchful Waiting vs. Gamma Knife for Small Symptom-Free Acoustic Neuromas
Patients with a smaller acoustic neuroma have typically been watched rather than proactively treated; the risks of early intervention have historically been thought to outweigh the benefits.
Enter an international study, led by UVA Health physicians and published in Neurosurgery (January 2025) that shows otherwise.
The findings of neurosurgeon Jason Sheehan, MD, et al., show that stereotactic radiosurgery (Gamma Knife) can prevent small tumors from growing over time, sparing patients from future potentially irreversible problems that can result from “watch and wait.”
Dr. Sheehan and his team performed a trial through the International Radiosurgery Research Foundation: 261 adults with the smallest category of acoustic neuroma or vestibular schwannoma.
Of the study subjects, 182 received stereotactic radiosurgery and 79 did not.
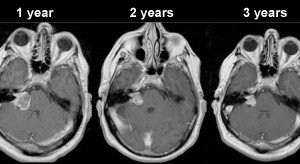
Those who underwent radiosurgery showed consistently better tumor control over time.
In this group, 99% of the tumors either remained the same size, grew just a little (less than 25%) or even shrank – at time intervals of three, five and eight years.
Only one participant’s tumor significantly increased in size.
Tumor control was much worse among those who didn’t receive the radiosurgery: 37% grew significantly at the three-year mark, 50% at five years and 67% at eight years.
For these patients with small acoustic neuromas that normally would’ve been only “watched,” radiosurgery was associated with a 54% reduced rate of tinnitus, a 51% lower rate of cranial nerve deterioration and 83% lower rate of vestibular dysfunction.
Notably, hearing was preserved similarly in both groups.
Dr. Sheehan says in the paper that acoustic neuroma symptoms are often irreversible as this tumor grows.
The paper says that early action, before symptoms develop, could considerably improve long-term quality of life.