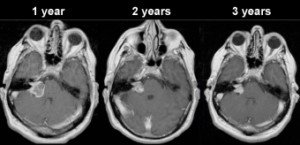
Because the cells of benign, slow-growing brain tumors divide slowly, the shrinkage effect of targeted radiation can take three years to show significant reduction in tumor size.
If you’ve been diagnosed with an acoustic neuroma…it IS possible that it’s really a meningioma.
A meningioma can be mistaken for an acoustic neuroma (aka vestibular Schwannoma).
Both of these conditions are slow growing brain tumors – though about two to three percent of meningiomas are actually malignant. An acoustic neuroma is never cancerous.
A person may become quite shaken up upon learning that their diagnosis of an acoustic neuroma has been changed to a meningioma.
Though a meningioma (along with its treatment) can lead to an array of permanent debilitations—depending on its location, of course—you must realize that if this mass has been mistaken for an acoustic neuroma, it and its treatment are not expected to cause permanent debilitations such as seizures, trouble concentrating or speaking, memory problems, personality changes or muscle weakness.
Thus, the fact that a meningioma can be misdiagnosed as an acoustic neuroma should not cause you to lose sleep.
How Does a Meningioma Get Mistaken for an Acoustic Neuroma?
“When a meningioma arises in the cerebellopontine angle or the internal auditory canal, areas that are more typically associated with an acoustic neuroma, they are sometimes confused for an acoustic neuroma,” says Gene Liu, MD, MMM, and Chief, Division of Otolaryngology, Cedars-Sinai Medical Group.
“The only times that a meningioma or acoustic neuroma would be confused with each other is if the meningioma is in the classic location for an AN,” continues Dr. Liu.
- Meningioma: abnormal growth of the meninges tissue that surrounds the brain and spinal cord.
- Acoustic neuroma: abnormal growth of the Schwann cells of the inner ear canal.
Does Treatment Change when an Acoustic Neuroma is Re-Diagnosed As a Meningioma?
“In these cases, the surgical approach for one lesion or another would not be any different (it’s based on location, not diagnosis),” says Dr. Liu.
“And whether or not the lesion was a meningioma or AN, the risks of the procedures are the same as well (because the risks are location/anatomy based, not diagnosis/pathology based — for these lesions)
“In the cerebellopontine angle or internal acoustic meatus, the surgical approaches would be to choose between a retrosigmoid (posterior fossa), middle fossa or translabrynthine.
“Each of these have different pros and cons. The choice of which boils down to — depending on size and location of the tumor — surgeon preference or expertise, preoperative hearing levels, etc. Yet the choice wouldn’t matter whether the lump was meningioma vs acoustic neuroma.
“So if you had one patient with a meningioma and another with AN, the surgical approaches and risks would likely be identical.
“Because of the location, symptoms cannot help to distinguish one lesion from the other.
“Both are benign; both are slow growing. The only way to tell one from the other is some potentially subtle differences on MRI scans.
“Thankfully, whether a tumor in these areas are meningiomas or acoustic neuromas, they are both monitored and treated in very similar ways.
“Although there may be some slight differences in the approach for a surgical procedure or the treatment regimen for radiation therapy, these differences tend to be very small and likely would not result in a big difference in outcome.”
Here is more information on the groundbreaking transcanal approach for the removal of an AN.