Heart failure can cause liver failure AND kidney failure, but what are the odds that the liver and kidneys decide to fail at the exact same time?
Is it more likely that heart failure injures the liver first, and then the liver injury causes a reduction in blood flow to both kidneys, thereby making both of them fail?
“Well, keep in mind that the basic (simplified) reason for liver failure in the context of heart failure is impaired perfusion or blood flow to the liver,” begins Mark Pool, MD, a board-certified cardiothoracic surgeon based in TX who’s been in private practice since 2011.
“May also be related to hepatic [liver] congestion from impaired blood flow through the heart — i.e., blood backing up into the lungs and all the way back to the liver.
“The mechanism for kidney failure in this context is usually also impaired perfusion.
“So, the heart is weak, not pumping enough blood to the kidneys, and the liver and the organs begin to fail.
“This can occur even if the blood pressure is low. Keep in mind that adequate perfusion is related to both the pressure and the volume of blood pumped.
“So, the BP can be sufficient but the volume of blood insufficient, if the ejection fraction is very low.”
Liver and Kidney Dynamics
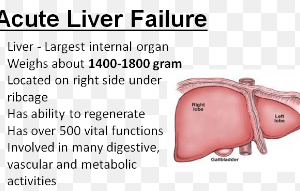
In some cases of chronic heart failure, the liver – having been struggling for a long time with reduced blood flow – just starts giving out, no longer able to function well with the poor blood supply.
The kidneys then follow suit. How do we know this in some patients? The precise pathogenesis of acute organ failure is often unclear.
But what if symptoms of acute liver failure are present in a chronic heart failure patient, yet during that time, their creatinine is at 2.5?
A 2.5 creatinine means poor renal function, but not poor enough to cause symptoms such as ascites (abdominal fluid buildup), appetite suppression, nausea and increased fatigue – which a liver that’s on the cusp of acute failure can easily cause.
The symptoms, though, can also be caused by a heart that’s entering acute decompensation.
But assume they’re being generated by the beginning of acute liver failure.
And within a few days, during which the symptoms have become more pronounced — including jaundice– the creatine has jumped to 3.2!
Hmmm, it seems as though acute kidney injury is in progress – triggered by the acute liver failure.
Indeed, dying liver cells can lead to backup in the vein that supplies the liver.
This creates a chain of events that culminates in constriction of the kidneys’ blood vessels.
With constricted blood vessels there will be reduced blood flow to these organs, leading to worsening renal function.
All of this is driven by poor cardiac output from chronic heart failure which, by now, may be in acute mode – caused by toxins in the general circulation that are reaching the heart.
The liver and kidneys are supposed to keep toxins, that all of us have in our bodies, quarantined.
But an injured liver can’t contain the toxins it’s supposed to process due to that backed up vein disabling operations.
The toxins end up outside the liver, all over the body.
The kidneys, failing miserably, can’t do their job of filtering toxins and filling the bladder with urine that contains these toxins to be excreted. Thus, there’s a growing toxin buildup in the body.
This damages the heart. The heart, now damaged more, pumps weaker than ever, and THIS affects the liver and kidneys…
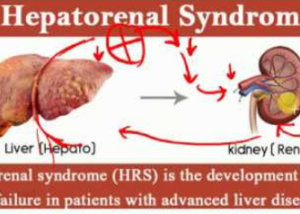
…all while the liver and kidneys are engaged in a vicious cycle of their own: hepatorenal syndrome.
Hepatorenal Syndrome
“My understanding of hepatorenal syndrome is that there is a feedback loop where impaired liver function gives rise to impaired kidney function, nearly independent of cardiac function, or at least, it can occur even in the context of a reasonably preserved heart function,” explains Dr. Pool.
“Certainly, low ejection fraction can amplify the effect. Both kidneys would likely be affected because this is a process related to perfusion.
“There could possibly be a stenosis [narrowing] of the renal artery, which would affect one kidney more than another; but in general, both kidneys would be expected to be affected with hepatorenal syndrome.”

Dr. Pool performs some of the most complicated and high-risk heart surgeries in North Texas, including redo operations and multi-valve surgery, and has performed over 3,000 major operations.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.