Is there a way to distinguish between a deadly prostate cancer and one that won’t kill?
What can be done to identify the lethal forms of prostate cancer?
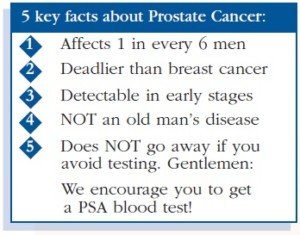
Prostate cancer kills close to 35,000 men every year in the U.S.
About 41 percent of newly diagnosed patients are between 65 and 74, while about 31 percent are 55-64, and a little over 7 percent are 45-54, according to the National Cancer Institute Surveillance, Epidemiology and End Results Program. Men 35-44 make up only 0.3 percent.
Though the five-year relative survival rate is over 96 percent, this figure includes early-stage diagnoses.
But stage 4 (advanced, spread to other organs) prostate cancer has a five-year survival rate of 28 percent, says Johns Hopkins Medicine.
So how can one tell the difference between a deadly prostate cancer and a survivable one?
“When a patient has signs and symptoms of prostate cancer, this typically indicates a prostate cancer that has progressed,” says Matthew Allaway, DO, a urologist who specializes in detecting prostate cancer and the developer of a prostate biopsy technique that improves cancer detection.
Dr. Allaway continues, “In general, prostate cancers that have progressed to the point of causing noticeable symptoms are more consistent with deadly rather than nonfatal prostate cancer.”
Though a prostate cancer may be growing very slowly, if left undetected it will eventually invade distant sites of the body, making long-term survival very difficult.
A diagnostic biopsy involves placing a needle into the walnut-sized prostate gland at standard locations or “cores.” MRI and ultrasound are sometimes used for visualization.
Usually there’s a dozen cores or locations where tissue is extracted for biopsy to check for the presence of cancer cells.
If cancer is present, a score, called Gleason, is assigned, based on the changes in glandular architecture.
A Gleason of 6 or less means a slow growing or indolent malignancy. A patient with a borderline Gleason score may still undergo surgery – which reveals a more aggressive cancer.
On the other hand, there are men with high Gleason scores whose surgery reveals indolent cancer.
A New Prostate Biopsy Technique
Dr. Allaway has developed an innovative technique for prostate biopsy that provides patients with a 30 percent better detection rate of malignancy, plus an almost zero percent infection rate.
Plus, there’s a reduced risk for pain, bleeding and urinary retention with this new biopsy method, which is called PrecisionPoint™ Transperineal Access System.
The trans-perineal path, through a single puncture of the skin, allows for a more thorough sample of all the regions of the prostate gland, including sections that are difficult to access via the standard trans-rectal approach.
The practitioner holds the instrument in his hand, which allows more precision, and the biopsy needle avoids the rectal wall – meaning, no potential for the transfer of fecal matter to the prostate, meaning very little risk of infection.
The trans-perineal method, done under local anesthesia, means the patient need not do any bowel preop or take pre-procedure antibiotics.
 Dr. Allaway is the founder and CEO of Perineologic, a medical device company focused on the development and delivery of technology to improve the safety, precision and efficiency of healthcare options in the field of urology.
Dr. Allaway is the founder and CEO of Perineologic, a medical device company focused on the development and delivery of technology to improve the safety, precision and efficiency of healthcare options in the field of urology.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.