What a real catch-22:
An elderly person on Coumadin takes a bad fall, but if you take them to the doctor this will result in a prescription cancellation for the blood thinner.
Your elderly parent is on coumadin (Warfarin) for stroke prevention. But they’re also at risk for falling.
Let’s take my very elderly father as an example. He uses a walker and is very unsteady with just a cane.
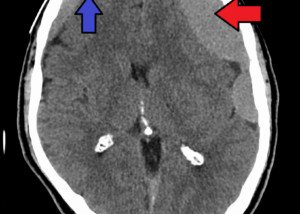
An elderly person on Coumadin who falls is at risk for internal bleeding – and this risk is substantial.
Even if they don’t strike their head, they can still end up with a brain bleed (simply from the jarring motion of the fall).
Studies have shown that physicians are hesitant to prescribe antithrombotic therapy [coumadin] in elderly patients with atrial fibrillation who are perceived to have an increased fall risk, to prevent inducing an intracranial hemorrhage. (NYU Langone Online Journal of Medicine)
I was SO relieved when my father’s medical team finally put him on Coumadin for stroke prevention.
His mother and sister had suffered a stroke. He has a-fib and not the best diet. These risk factors plus his advanced age are just screaming for a stroke.
He frequently has “balance adjustments,” as he calls them, often wobbling and re-steadying himself by grabbing a kitchen counter or door frame.
And he’s almost fallen several times but was saved by tipping into a stable object that blocked what would have been a solid fall, such as a sturdy stack of heavy boxes.
Recently he fell after my mother, standing before him, lost her balance when picking something up. She fell into him, causing him to fall to the ground.
At the ER (his ankle was very swollen) he told the doctor he fell after losing his footing on a step. My mother was with him and did not want the truth revealed.
Several days later my father visited his primary care physician for follow-up, who was part of the team who prescribed the Coumadin.
When asked how the fall occurred, my father told the truth this time (my mother was not present).
Not long after that, the doctor explained that had there not been any extraneous factor causing the fall, the coumadin prescription would have to be cancelled.
“I will take you off Warfarin,” asserted the doctor with passion in the event of any future fall that was not caused by someone else.
Do you have a similar situation with an elderly family member?
An elderly person on a blood thinner who falls, even if they claim “I’m fine,” should be taken to the ER just to make sure there are no signs of internal bleeding or a small fracture somewhere.

Freepik/rawpixel.com
On the other hand, if we keep silent, then internal bleeding could be festering, building up over several days, then reaching a critical point where it suddenly causes severe symptoms and is then—ultimately—non-retractable, resulting in death.
But if the patient sees a doctor in the name of making sure everything is alright, they risk getting the coumadin prescription revoked.
This means anxiety over a high risk of stroke.
Several hours after the follow-up visit, my father fell in the kitchen – but I just happened to be in the doorway near him (he didn’t know this due to the angle) and I caught him by the arm and shoulder!
Talk about a catch-22! Shall we report the next fall if there’s no apparent injuries, knowing full-well there COULD be slow internal bleeding?
Should you tell doctor of a fall and risk cancellation of blood thinner prescription?
However, elderly patients [with atrial fib] who are deemed at risk of falls are often not started on warfarin therapy secondary to a perceived higher risk of bleeding complications.
These risks have been evaluated, but conclusive data regarding risk-benefit trade-off are elusive. (American Heart Journal, 2011 Feb;161(2):241-6)
There is a general tendency among physicians to underuse anticoagulants in the elderly, probably both because of underestimation of thromboembolic risk and overestimation of bleeding risk.
Assessing the benefit-risk ratio of anticoagulation is one of the most challenging issues in the individual elderly patient. (Journal of Clinical Interventions in Aging, 2009; 4: 165–177)
The decision to anticoagulate an elderly person with AF at high risk for stroke is a common problem faced by physicians. (NYU Langone Online Journal of Medicine)
Should you report the fall (when the patient declares they “feel okay” and there are no visible signs of injury) and risk your elderly family member with AF (and other stroke risk factors) being taken off the blood thinner?
Or should you keep silent and pray that a slow brain bleed or abdominal bleed isn’t in the works? Or that a subtle fracture didn’t occur?