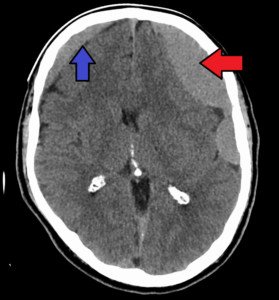
A chronic subdural hematoma is a very slow bleeding in the brain.
Just when you thought you were in the clear for having a brain injury, this kind of bleeding could rear its ugly head.
In fact, a CAT scan taken 24 hours after getting hit in the head may be perfectly normal, and then weeks go by without any problem, and then one day the patient awakens with symptoms: a chronic subdural hematoma is at work.
How Long It Takes for Symptoms of Chronic Subdural Hematoma to Start Showing
I wondered if there was a “grace period” during which the symptoms of chronic subdural hematoma would present, and then if there was a period of time following getting hit in the head, that if a patient still didn’t have symptoms, he could rule out chronic subdural hematoma.
Obviously, the hit that I took on my head two years ago, to this day, has not produced any symptoms.
So I can safely assume that I currently don’t have a chronic subdural hematoma, even though in theory, I could have developed a very small one without symptoms several weeks after the trauma, which resolved on its own.
But is there a grace period?
“There is no good answer for this question, as symptoms will be very dependent on a number of factors such as the age of the patient, variability with the amount of atrophy, the degree/severity of the trauma, history of other risk factors such as anticoagulant use, etc.,” explains Kangmin Daniel Lee, MD, a neurosurgeon with New Jersey Brain and Spine.
Old age is a major risk factor for chronic subdural hematoma, though younger people can get these as a result of blunt trauma to the head.
In fact, young children are more likely to get a chronic subdural hematoma from head trauma than young adults or middle aged adults.
Combine old age with daily use of anticoagulants such as aspirin or Coumadin, and you up the ante for the risk of developing a chronic subdural hematoma if the person hits his head as a result of a slip-and-fall, or bumps his head when getting into a car, or strikes his head on the underside of a table after being on all fours searching for a dropped coin.
“The average length of time between head trauma and presentation to the emergency room is typically one month in the case of chronic subdural hematoma.
“This is likely due to the slow and progressive nature of symptom onset. The age of the hematoma is easily confirmed by observing the density of the blood on CT scan.”
If you hit your head, or get hit in the head, even if it doesn’t cause immediate symptoms like a headache or dizziness, you still should take note of the date it happened.
The reason is … you may feel fine for several weeks, then awaken one day with out-of-the-blue symptoms, like my mother did:
A headache that she described as feeling like a “crown of thorns” that wouldn’t respond much to painkillers; significant leg weakness (one leg more so than the other) that made it nearly impossible for her to stand up from a chair; and upchucking.
This occurred six weeks after she lost consciousness from a blood pressure drop while standing, and fell dead-weight against the bathtub, striking her head. The diagnosis was a chronic subdural hematoma.
Just one week before the sudden onset of the symptoms, my mother had attended an exercise class and reported that it was too easy for her!
Chronic subdural hematoma is a very stealthy condition, and if symptoms appear, you absolutely must seek medical treatment.
 Dr. Lee focuses on minimally invasive techniques to treat traumatic and degenerative diseases of the spine and brain tumors. He’s been invited to speak at the regional and national levels on his research areas.
Dr. Lee focuses on minimally invasive techniques to treat traumatic and degenerative diseases of the spine and brain tumors. He’s been invited to speak at the regional and national levels on his research areas.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.


























