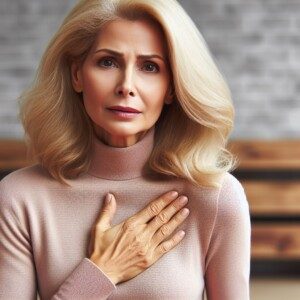
Imminent heart attack can be missed by ER doctors when it comes to your chest pain.
The ER doctor may misdiagnose your chest pain as GERD or acid reflux.
My mother went into the ER with chest pain and shortness of breath, and the ER doctor thought it was GERD after the second troponin test (like the first) came back normal.
A heart attack releases troponins – a protein that leaks from injured cardiac tissue – into the bloodstream.
He actually told my mother, “I don’t think you have a heart problem. This has a GI flavor to it.” Yes, exact words.
The ER doctor prescribed Prilosec, a heartburn drug. Less than 48 hours later, my mother was undergoing quintuple bypass surgery.
What on earth happened?
“The patient is probably having pain from ischemia (angina), but since there has been no tissue death, troponin won’t appear,” says Christopher J. Hanifin, PA-C, who was previously a physician assistant in open heart surgery with Cardiothoracic Surgery of South Bend in South Bend, IN.
“In theory anginal pain can come and go almost indefinitely, so these folks can have hours of pain with negative tests,” continues Hanifin.
“It’s just a matter of timing when the tissue finally starts to infarct [dies from obstructed blood supply]. Unfortunately for some folks, this is not until after discharge.”
# 1 depicts a blood clot. JHeuser [CC BY-SA 3.0]
Misdiagnosis of a Pending Heart Attack for GERD
My sister is a medical doctor. She flipped when I told her the ER doctor diagnosed our mother’s chest pain and shortness of breath as acid reflux.
My sister fumed, “Chest pain is so often misdiagnosed as GERD and patients are sent home and then have a heart attack!”
My mother didn’t have the heart attack. Two days later she was back in the ER with chest pain, and this time, a different ER doctor recommended she be admitted because her troponin level was elevated – not enough to diagnose heart attack, but enough to concern the ER doctor.
“When looking at a test like cardiac enzymes, it is important to consider that it is not really testing whether a patient is HAVING a heart attack,” says Hanifin.
“It is testing whether a patient HAD a heart attack over the previous several hours to days.”
The test does not tell if your arteries are clogged.
There was no further chest pain during her evening and overnight hospital stay, and even next day, no chest pain.
An echocardiogram was performed first (the next day) to see if it was safe to have a stress test.
The echocardiogram came back “abnormal,” and the cardiologist recommended the invasive catheter angiogram.

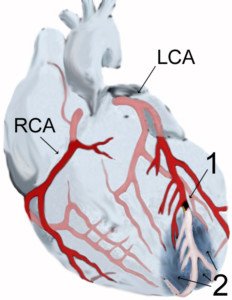
Catheter angiogram is the gold standard for detecting blocked arteries, but it comes with the risk of stroke and heart attack — though this risk is very small. Shutterstock/MAD.vertise
“It’s unsafe to send you home,” the internal medicine doctor told her after she insisted she wanted to just go home.
All along, I had felt funny about that first ER diagnosis of GERD.
That first visit hadn’t been just for chest pain and shortness of breath.
My mother had also vomited that morning. The triad of chest pain, shortness of breath and vomiting can mean an imminent heart attack!
However, the first ER doctor was all too sure that the chest pain, shortness of breath and vomiting meant GERD.
What should’ve the first ER doctor told my mother?
He should have explained: “The negative troponin means you did not have a heart attack. We did not give you a diagnostic test for GERD — and this may very well be GERD, but … we also did not give you any tests to rule out severe heart disease, either.
“Though your symptoms sound like GERD, they also sound like extensive coronary artery blockage. I can’t send you home with a diagnosis of GERD.
“I am going to send you home with a diagnosis that you did not have a heart attack. But I can’t rule out that you won’t have a heart attack in the next 24 hours.”
The catheter angiogram revealed extensive coronary artery blockage, and the bypass surgery was begun only a few hours later.
Prior to surgery, I had asked the cardiothoracic surgeon, cardiologist and internal medicine doctor these exact words: “You mean, if my mother goes home without this surgery, she might have a fatal heart attack within a week?”
All three simultaneously said yes. That is the truth.
“Making medical decisions involves looking at probabilities,” says Hanifin. “A chest pain patient who has multiple negative cardiac enzymes, ECGs and a negative stress test has a very small likelihood that their pain is due to ischemia, but the likelihood is never 100% eliminated.”
Another issue is that emergency rooms do not provide stress tests.
The patient would either have to be admitted to get a stress test the next day, or, if the patient is sent home from the ER, it could be many days before they could get a stress test scheduled through their doctor. By then it could be too late.
“The decision to further evaluate a patient is therefore based on a person’s risk factors,” says Hanifin.
“Factors like diabetes, high blood pressure, smoking, a sedentary lifestyle and a family history of cardiac disease are all very troubling in a chest pain patient, even when their tests look good.”
 Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
Christopher J. Hanifin, PA-C, is currently Department Chair and Assistant Professor, Department of Physician Assistant, Seton Hall University, NJ.
 Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, health and personal security topics for many years, having written thousands of feature articles for a variety of print magazines and websites. She is also a former ACE-certified personal trainer.
.