Every year, about 100,000 people visit their doctor with abdominal pain, and around 30,000 of these are diagnosed with gallstones.
For many, the standard treatment has been laparoscopic cholecystectomy, a surgery to remove the gallbladder.
Since the 1990s, this surgery has become increasingly common, even though there’s no clear international guideline on when it’s most appropriate.
In the Netherlands, gallbladder removal has become one of the most frequent surgeries, but it doesn’t always solve the problem: About a third of patients still experience abdominal pain afterward.
This has raised concerns about the appropriateness of the procedure, although things are starting to change.
A Study on the Necessity or Not of Gallbladder Removal
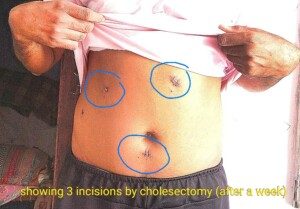
Three incisions for a gallbladder removal. Credit: Shemaroo, CC BY-SA 4.0/creativecommons.org/licenses/Wikimedia Commons
A 2019 study from Radboud University Medical Center looked into this issue by dividing patients with abdominal pain from gallstones into two groups.
One group underwent the usual cholecystectomy, while the other group followed a more selective approach.
This means surgery was only considered after a thorough review of their pain symptoms.
The study found that the selective approach led to fewer surgeries, but one year later, a third of patients in both groups still had pain.
This prompted researchers to advise caution when considering cholecystectomy for patients with gallstones and abdominal pain.
A recent follow-up study, published in JAMA Surgery, revisited these patients five years later.
Daan Comes, the lead author of the study, explained, “We wanted to see long-term effects of using a selective strategy for this surgery.”
He continues, “We reached out to over a thousand patients by phone, had them fill out questionnaires, and reviewed their medical records.”
The results showed that the rate of pain hadn’t significantly changed: about two-thirds of patients were still pain-free.
However, the selective approach did result in fewer unnecessary surgeries.
No more complications were observed in the selective group compared to the usual surgery group, indicating that this approach can be effective if used with the right patients.
To better identify who might benefit most from surgery, Radboudumc developed a decision rule in 2021.
According to Dr. Philip de Reuver, who led this effort, intense, episodic pain is a strong indicator that surgery could be beneficial.
However, if a patient has had previous abdominal surgery or has additional symptoms like bloating, heartburn, or ongoing pain, doctors should be cautious about recommending surgery.
With this new information, doctors and patients can make more informed choices.
De Reuver explains in the research paper that those with a recurrent biliary colic can certainly benefit from the surgery.
Many with gallstones, though, also have acid reflux and IBS, and surgery will not fix these conditions.
Thus, other issues must be ruled out before proceeding with the surgery.
To further improve patient outcomes, De Reuver is launching a new study on how lifestyle changes might help those with abdominal pain and gallstones where surgery might not be the best option.
He hopes that lifestyle adjustments will improve health, quality of life, and reduce pain.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.










































