How could it be possible for a physically fit person in middle age to have significant coronary artery disease: dangerous blockages in their heart’s arteries?
There are middle age men and women who, upon being informed that they need a coronary bypass surgery or that they have a non-emergent case of clogged arteries, have reacted with any of the following:
- “But I’ve always eaten healthy!”
- “I’ve always been very active! I’ve been working out at a gym for years; I ski; I hike.”
- “But I’ve never smoked; I hardly drink!”
- How could this be? I’ve never been overweight, I watch my sodium intake and I’ve always had low blood pressure!”
Blockages in the coronary arteries is an extremely common occurrence, and it often causes no symptoms.
When it does, though, these include the classic chest pain and shortness of breath – occurring from easy activities that previously had not caused these symptoms.
As coronary artery disease (CAD) progresses, chest pain and feeling unusually winded or short of breath may occur at rest.
A middle age person who believes they’ve been doing “everything right” may still end up with substantial blockages (occlusions) in their coronary arteries, requiring treatment.
How does this happen?
“Family history — The first thing I would look for is someone with a family history of premature heart disease,” begins Alexandra Kharazi, MD, a cardiothoracic surgeon with CVTS Medical Group, Inc., Chula Vista, CA.
“This can often be hereditary. For example, familial hyperlipidemia [excess fat in the blood] is a condition which can be passed down and predispose to heart attacks at an early age.”
Why did humans evolve to suffer from a hereditary-driven CAD?
After all, isn’t evolution supposed to be efficient and not make mistakes?
Aren’t all the species of animals out there supposed to have evolved to be perfectly adapted to their environment?
You’d think so. But modern medicine has eliminated the need for humans to evolve healthy sturdy hearts that could hold up until ripe old age.
With all sorts of medical interventions, people with very sick hearts could live many years in that condition.
Thus, the evolutionary premise of “Survival of the fittest” does not apply to the human species.
The genetic basis for premature heart disease is rampant in the human genome.
But we must also consider environmental factors, as in: “Genetics load the gun, but environment pulls the trigger.”
Dr. Kharazi says, “There are several risk factors for heart disease, most commonly hypertension, hyperlipidemia, diabetes, smoking, obesity.”
Hypertension (high blood pressure) is lifestyle-driven, though some individuals are blessed with a genetic profile that keeps their blood pressure in the normal or even low range despite some unhealthy lifestyle choices.
Excess fat in the blood is also primarily driven by lifestyle, though a genetic predisposition can make it more difficult to get this under control.
Type 1 diabetes can strike anyone, but type 2 diabetes is driven by unhealthy lifestyle habits, mainly obesity.
Needless to say, the choice to smoke has no genetic component.
Though some people gain excess weight more easily than others, carrying around significant excess weight is the result of lifestyle choices.
Yes, some conditions cause fat gain, but these conditions, such as polycystic ovarian syndrome and underactive thyroid, do not cause someone to be 100 pounds overweight.
The rate of obesity in the U.S. has skyrocketed since the 1970s. This is not due to genetics, medical conditions or drugs that can cause weight gain.
“However, not all of these have to be present, and sometimes one is predominant over others,” says Dr. Kharazi.
“This can mean someone isn’t necessarily aware they have high blood pressure, for example, and therefore may not think they need to see a doctor for a routine checkup which may diagnose heart disease.”
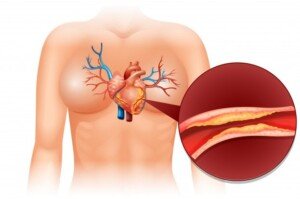
Plaque buildup narrows a coronary artery. A piece of soft plaque can break off and trigger a clotting response, blocking oxygen to the heart: a heart attack. Freepik.com/brgfx
Are you SURE you’ve been “doing everything right”?
Another point to consider is the possibility that the patient’s lifestyle isn’t as “healthy” as they think it’s been.
Many people also overestimate their level of fitness. They look in the mirror, see a trim waistline and automatically assume they have a healthy heart.
Certainly, trimness has no negative effect on the heart, and obesity is always bad for it – either directly or indirectly (causing conditions that damage the heart).
But if you haven’t been exercising much, how could your heart be strong and know how to efficiently recover from physical exertion?
- The heart is a muscle.
- It can only get strong from exercise.
Exercise also trains the body to efficiently extract oxygen from blood cells. Structured aerobic activity improves cardiovascular health.
The older one gets, the more important it is to exercise for heart health – even though youth is never a reason to avoid consistent cardiovascular workouts.
You aren’t necessarily in “great shape” just because your build is slender, you don’t smoke and you’re middle age rather than over 65.
The cardiac muscle needs regular, structured exercise that keeps heartrate elevated.

Shutterstock/Oscar Carrascosa Martinez
Gender
Dr. Kharazi explains, “Women are more likely to present with ‘atypical symptoms,’ as opposed to the classic presentation of chest pain, and therefore diagnosis may be delayed.
“Sometimes, women (particularly who are diabetic) have no symptoms at all until plaque buildup is critical.”
You May Have a Family History of Poor Heart Health and NOT Know It
Dr. Kharazi confirms that she’s had coronary bypass patients who, by appearance alone, seemed to be in excellent physical condition (V-shaped build, toned muscles, no potbelly) – and it wasn’t just a matter of how they looked.
These patients did report vigorous activities on a regular basis. She says, “Usually, they have a strong family history.”
The absence of a family history of CAD does not give you a green light to load up on salty processed foods and hardly get any systematic exercise.
Furthermore, you simply do NOT know if there’s an absence of family history anyways.
For example, suppose your father passes away from prostate cancer at 65.
But what if he had never gotten the cancer? How do you know if, all along, plaque wasn’t building up in his coronary arteries?
Maybe had he not passed from the cancer, three of his main coronary arteries would’ve ended up 98% blocked by the time he was 67.
And maybe at 68, he would’ve started having chest pains, ignored, them, then had a fatal heart attack at 69.
Plus, there’s always the possibility that in this hypothetical scenario, Dad could’ve made it to 90 without medical intervention despite having severely occluded coronary arteries. Sometimes it’s just a roll of the dice.
People die from all sorts of causes including car accidents and pneumonia.
Just because your parent or grandparent dies from a non-heart related cause doesn’t mean they didn’t have CAD.
So what’s the takeaway?
• Middle age doesn’t protect you from dangerous plaque buildup.
• Whether you smoke, have a junk food diet or are overweight, you STILL can make a difference in your heart’s health by committing to consistent aerobic exercise. Adding strength training would even be better!
• However, a faithful exercise program is no reason to keep smoking, keep eating a lot of ultra-processed foods and not work on losing excess fat.
• If you have a family history of CAD or heart attacks, speak to your doctor about when you should begin annual heart health exams.
• If you don’t have a (known) family history, you should start getting annual cardiac health checks at 45.
 Dr. Kharazi has many areas of surgical expertise including the following: aortic aneurysm repair, aortic valve repair and replacement, and CABG. Other areas of focus include arrhythmia, bloodless medicine, lung cancer and resection, septal defect repair and thoracic surgery.
Dr. Kharazi has many areas of surgical expertise including the following: aortic aneurysm repair, aortic valve repair and replacement, and CABG. Other areas of focus include arrhythmia, bloodless medicine, lung cancer and resection, septal defect repair and thoracic surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.



























