Have you gone four days without a BM?
What if going four days without pooping is a common occurrence?
Does it make a difference if when you finally go, your bowel movements come out easily vs. you must strain?
You may have read online or even in a pamphlet that people should have a bowel movement every day.
This is a common guideline and can really scare people who routinely go two or three days without a bowel movement.
It can be especially worrisome for those who, from time to time, go four days without a poop.
If going four days without a BM is a recent occurrence that has happened only once, this will be even more concerning to the health conscious individual.
You may have also read another version of the normalcy of pooping: It should occur “at least three times a week.”
Again, this excludes once every four days.
But should you really worry if, from time to time, four days go by without a BM?
What if this has recently happened, and hence, there is no lengthy time passage of otherwise good digestive health, following the situation, to reassure you?
You’re then left wondering if this four-day span is going to keep occurring, or if soon you’ll be seeing blood in your stools or having stomach cramps.
On the Fifth Day, You Finally Had a Poop
“Four days without a bowel movement usually does not indicate a serious medical condition,” says Supriya Rao, MD, a quadruple board-certified physician with Integrated Gastroenterology Consultants.
“That being said, it could indicate something is wrong. If you go longer than four days and think something’s up, consult with your physician.
“The most common causes of irregular bowel movements are dietary changes, inadequate fiber intake and dehydration.
“Other causes could include stress, side effects from certain medicines or medical conditions such as irritable bowel syndrome (IBS), inflammatory bowel disease (IBD) and malabsorption syndromes.”
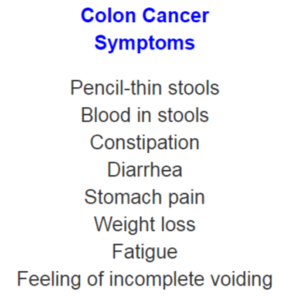
What about colon cancer?
That’s the big question. If you’ve gone four days without a BM, and your imagination is on the active side, you may begin visualizing a tumor in your lower colon – blocking feces from getting past it and out your anus.
But then on that fifth day, the cancer shifts position and lets the backed-up fecal matter through.
However, this is an unlikely scenario. A malignant tumor will be securely fixed in place.
It’s not going to completely block feces one day, then let it through the next because it somehow shifted out of position.
Nevertheless, a tumor often will partially block stool matter – making it come out in ribbon or pencil shapes.
If, after your four day hiatus from bowel movements, you resume passing stools the way you normally do, this makes even LESS the case for a growing colon cancer.
Now, if going four days without a BM ultimately becomes your new normal, you should definitely take a look at your stools and also be aware of any new symptoms such as unexplained fatigue, weight loss and especially blood in the stool.
If you don’t have any of these other symptoms, you should still see a gastroenterologist.
- If any physician ever says, “You’re too young to have colon cancer,” get a second opinion.
- Colon cancer CANNOT be ruled out without a colonoscopy.
- People under 40 do get colon cancer, though it’s rare in this age group.
If you’re reluctant to do that, for whatever reason, you should at least keep a record of your BMs to see if there’s a common thread with the four-day lapses – such as a food binge paired with unusually low levels of physical activity.
Relief of Constipation
“To help with constipation and being backed up, make sure to stay hydrated and increase your fiber intake if possible (the single most important thing to improve gut health),” says Dr. Rao.
Aim for 25 grams of fiber a day. High fiber foods include lentils, beans and fruit, especially berries.
“To get things moving, eat prunes, drink warm liquids such as warm lemon water or take a stool softener.”
Move more, too. Being sedentary can lead to constipation. Get up and about more.
And avoid binge eating. This could lead to impaction of hard stools that may require a doctor to manually pull out.
“If your constipation persists or you experience other symptoms such as abdominal pain, bloating, nausea or vomiting, it’s important to contact your healthcare provide,” says Dr. Rao.
 Dr. Rao is board certified in internal medicine, gastroenterology, obesity medicine and lifestyle medicine. She is managing director of Integrated Gastroenterology Consultants, and director of Medical Weight Loss at Lowell General Hospital. She also runs the motility program, which focuses on disorders of the esophagus, irritable bowel syndrome and anorectal disorders.
Dr. Rao is board certified in internal medicine, gastroenterology, obesity medicine and lifestyle medicine. She is managing director of Integrated Gastroenterology Consultants, and director of Medical Weight Loss at Lowell General Hospital. She also runs the motility program, which focuses on disorders of the esophagus, irritable bowel syndrome and anorectal disorders.
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.



























