There are cases in which a chronic subdural hematoma on a CT scan image is missed.
How can this be?
“In general, some subdural hemorrhages can be particularly hard to see on CT because, as they age, their density can become almost the same as the surrounding normal cerebrospinal fluid,” says Resham Mendi, MD, a renowned expert in the field of medical imaging, and the medical director of Bright Light Medical Imaging.
“When the density is similar (isodense), the blood can blend with the adjacent normal fluid,” says Dr. Mendi.
I am reminded of a man I met at the gym who was in his late 60s. I noticed that one side of his body was disabled, though he was able to walk without assistance.
He made a comment on my lift, which then opened the door to me asking what had caused his disability.
He told me he’d fallen backwards while sitting in a chair at a computer and slammed his head on the floor.
About 30 days later he began having concerning symptoms, went to the ER and had a CT scan of his head. It came back normal.
However, the symptoms only grew worse, and about 30 days after the first CT scan he had another, and this time it showed a chronic subdural hematoma.
When that second CT scan was compared to the first, the bleeding was only then identified on the first image.
At that point it was established that whoever read the first CT scan had missed the chronic subdural hematoma.
As a consequence of delayed treatment (which would have entailed surgical draining of the excess fluid), the man suffered permanent mobility problems on one side of his body.
There is no data on what percentage of CT scans for a suspected chronic subdural hematoma are missed.
But there are times when they are missed in symptomatic patients.
Patient Has Recent Fall History, Current Neurological Symptoms
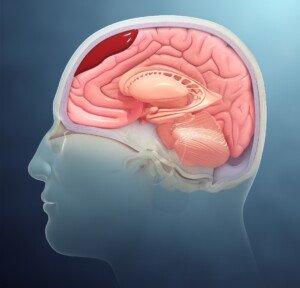
The collection of fluid will make the natural convolutions (burrows) of the brain less clear on the image.
So if the classic crescent shape of the bleed is not obvious, the more faded area of the convolutions should be – which should then be a tipoff to the radiologist that there is a very slow brain bleed in that area – especially when other possible causes of the symptoms have been ruled out.
A chronic subdural hematoma is a slow bleeding under the dura mater of the brain, and it can take up to 90 days before the first symptoms begin appearing.
Symptoms include headache, one-sided weakness, dragging one foot when walking, slurred speech, cognitive changes and seizure.
In an acute SH, the symptoms occur within 24 hours of the head trauma, often instantly or soon after (high mortality rate). Loss of consciousness may be instant or within hours.
There may also be projectile vomiting (highly suspicious for acute bleeding), a searing headache, increasing drowsiness and seizures.
If you suspect you or a family member have a chronic subdural hematoma, but the CT scan comes back negative —
— you should request an MRI, which is more sensitive to showing the collection.
Also keep in mind that if the person’s head did NOT hit anything during a fall, this does not rule out the possibility of a brain bleed.
The jerking motion of the head in an elderly person, even though the head does not hit anything, is sometimes all it takes to tear tiny veins and cause the slow leaking of blood.
Dr. Mendi has published several articles in radiology journals and has expertise in MRI, women’s imaging, musculoskeletal, neurological and body imaging.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.