In plain English which is better for acoustic neuroma treatment: radiosurgery (pinpointed radiation on the tumor) or “under the knife” surgery in which the tumor is cut out?
If you’ve been diagnosed with an acoustic neuroma, you may already know that there are three main treatment options (besides surveillance):
• Radiosurgery (“cyber knife,” “Gamma Knife” or targeted radiation)
• Regular surgery (microsurgery)
• Transcanal surgery (not as common)
Karpinos et al made a comparison between radiosurgery and regular surgery for acoustic neuroma in 96 patients.
Gamma Knife vs. Surgery to Treat Acoustic Neuroma
• Between 1993 and 2000 the subjects were treated at Memorial Hermann Hospital, Houston.
• Subjects who had regular surgery had larger tumors and were younger when compared to the Gamma Knife group.
• Tumors were divided into small, medium and large.
Tumor Growth Control After Treatment
• 100 percent for regular surgery
• 91 percent for Gamma Knife
Measurable Hearing Preservation
• 57.5 percent for Gamma Knife
• 14.4 percent for regular surgery
Facial Neuropathy (problem with facial nerve)
• Development of facial neuropathy in the surgery group was “significantly higher” than in the radiosurgery patients.
Trigeminal Neuropathy (problem with cranial nerve)
• You guessed it: The surgery group had a “significantly higher” rate of neuropathy.
Miscellaneous
• Microsurgery patients had a longer hospital stay.
• Microsurgery patients had more perioperative complications (this means during and post-operative phases taken together).
The full report is in International Journal of Radiation Oncology (12/2002).
Conclusion
“The decision of whether to observe versus operate versus perform radiosurgery (Gamma knife) is complex and dependent on the patient’s age, symptoms (balance issues and hearing), tumor size and characteristics, and patient’s values,” says Ted McRackan, MD, MSCR, Director, Skull Base Center; Assistant Professor, Department of Otolaryngology – Head and Neck Surgery, Medical University of South Carolina.
“The patient should discuss all options with his or her treating physician.” There is no one-size-fits-all template.
Acoustic Neuroma Risk Factors
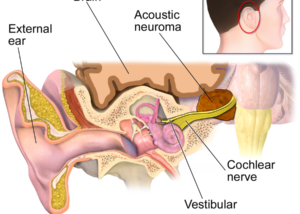
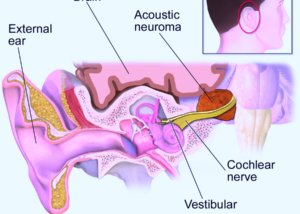
One primary risk factor for this benign tumor of the inner ear is genetic predisposition.
Individuals with a rare genetic disorder called neurofibromatosis type 2 (NF2) are at a significantly higher risk for developing acoustic neuromas.
NF2 is an inherited condition characterized by the growth of noncancerous tumors on nerves, including those associated with hearing and balance.
Another potential risk is exposure to environmental factors, though this connection is less well-established.
Some studies suggest that prolonged exposure to certain environmental toxins or radiation may play a role in the development of acoustic neuromas, but more research is needed to confirm these links.
Age and gender also influence risk. Acoustic neuromas are most commonly diagnosed in people between 30 and 60, and they tend to occur slightly more frequently in women than in men.
However, the reasons for these demographic patterns are not yet fully understood.
 In addition to acoustic neuroma, Dr. McRackan’s clinical practice focuses on comprehensive management of ear, hearing, balance and skull base disorders. Areas of interest include cochlear implants, facial nerve disorders and tumors, vertigo and endoscopic ear surgery.
In addition to acoustic neuroma, Dr. McRackan’s clinical practice focuses on comprehensive management of ear, hearing, balance and skull base disorders. Areas of interest include cochlear implants, facial nerve disorders and tumors, vertigo and endoscopic ear surgery.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.