
Pronator syndrome can cause painful symptoms in the hands and forearms that mimic carpal tunnel syndrome.
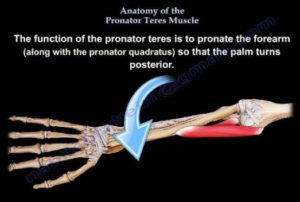
Pronator syndrome is when the pronator teres muscle of the forearm presses upon the median nerve, the same nerve that’s involved in carpal tunnel syndrome.
Pronator teres syndrome is a nerve entrapment condition. The median nerve gets compressed by the pronator teres muscle; the median nerve is located beneath the superficial head of this forearm muscle.
“Activities involving repetitive wrist and forearm movements are thought to increase the risk of developing pronator syndrome,” says Jonathan Oheb, MD, North Valley Orthopedic Institute, Chief of Orthopedic Hand and Upper Extremity Surgery.
“Pronator syndrome occurs secondary to increased pressure on the median nerve in the forearm.
“These repetitive motions can lead to muscle hypertrophy and/or swelling, increasing the pressure over the nerve as it travels through the forearm.
“This is often in conjunction with a patient’s underlying anatomy which may predispose them to developing this in the first place.”
As a former personal trainer, I’m very familiar with the pronator muscle (reverse arm curls target it).
This muscle is responsible for the wrist joint action of pronation, i.e., turning the forearm over so that the palm faces downward or behind you, depending on where your hands are in space; or, if the hands are elevated, turning the palms facing away from you (as in a pull-up).
Though the compression site is in the upper forearm, the symptoms will not only be felt in this area, but also will affect the hand and fingers.
The median nerve controls movement and sensation in most of the hand.
When you want to move your thumb, for instance, a signal from the motor control region of your brain travels down your neck to the median nerve, which extends from the neck region (spinal cord) and runs the entire length of the arm, with its final distribution to most of the hand, including the thumb.
The electrical nerve impulse signal, that originated from your brain, will zip down the median nerve all the way to the thumb, where the nerve distributes to thumb muscles.
The electrochemical impulse will cause the thumb muscle to contract: You just moved your thumb. These nerve signals travel about 50 meters per second.
If the median nerve is compressed somewhere along the way, some of the nerve signal from your brain will never get past the compression point, and hence, why movement in the fingers can be limited or “stiff.”
Numbness is also a symptom for the same reason in reverse:
Sensory neurons normally send signals up the median nerve to the sensory interpretation center of the brain.
If there is a blockage of these signals at the compression site, all the signals won’t make it to the brain, and hence, numbness, rather than a full sensation of feeling.
In addition to compromised motion and numbness, pronator syndrome also causes pain, including in the hand.
The median nerve distributes to the thumb, index and middle fingers, and the half of the fourth finger that faces the middle finger.
Face your right palm towards you. Imagine a line running down lengthwise the fourth finger, dividing it in half. Continue “drawing” that line all the way to the wrist.
Now, imagine shading the portion of your hand and fingers to the right of this imaginary line. This is the area impacted by pronator syndrome.
In other words, the other longitudinal half of the fourth finger, plus the entire pinky and outer portion of the palm, are not affected.
Nevertheless, these symptoms can also be caused by carpal tunnel syndrome, despite what you might have read or will read. Wrist motions should not aggravate pronator teres syndrome symptoms.
Misdiagnosis
A chiropractor misdiagnosed my mother with pronator teres syndrome based on questioning her and feeling her arm for pain triggers.
Then an ER physician misdiagnosed her; he suspected nerve compression at the neck and ordered an MRI. The MRI showed cervical disc degeneration and he said, “It’s what I suspected: nerve compression of the neck.”
The most definitive test to rule in or out nerve entrapment conditions is the EMG test.
An EMG test ruled out cervical compression and pronator syndrome in my mother, and solidly confirmed carpal tunnel syndrome.
Interestingly, the neurologist who performed the EMG test, prior to the test, was very convinced she had pronator syndrome.
But an EMG test does not lie. It revealed a nerve signal conduction blockage at the wrists of both hands: carpal tunnel syndrome.
Treatment
Treatment for pronator syndrome may consist of simply massage.
A chiropractor might be convinced that chiropractic manipulation can correct the problem over a number of visits.
If conservative treatments aren’t successful, then surgery is a final resort.
Prevention
Dr. Oheb explains, “Ways to reduce the risk of developing pronator syndrome mostly involve proper warm-up and stretching before strenuous activity.
“Also, maintaining good strength and flexibility through regular exercise can be preventative.”
 In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
In addition to hand, elbow and shoulder care, Dr. Oheb provides comprehensive surgical and nonsurgical treatment for all orthopedic conditions of the hip, knee and ankle, including broken bones and injuries. jonathanohebmd.com
 Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
Lorra Garrick is a former personal trainer certified through the American Council on Exercise. At Bally Total Fitness she trained women and men of all ages for fat loss, muscle building, fitness and improved health.
.









































