Melanoma can arise from a pre-existing mole, so you might be thinking that it’s smart to have your normal moles removed to at least prevent the development of melanoma from these moles.
If you have many moles, the idea of having them electively removed will be even more appealing, since having many of these skin lesions is one of the risk factors for melanoma.
Having moles electively removed, out of melanoma fear, can also be referred to as “de-moling.”
However, “The principal always followed in medical care is according to Hippocrates’ oath, ‘First do no harm,’” says Maria M. Tsoukas, MD, PhD, Assistant Professor, Dermatology Section, University of Chicago.
In medicine and specifically in dermatology, we keep a very low threshold in clinical examination and in deciding which nevi need to be biopsied or removed.”
A nevus is the Latin term for mole, and nevi is the plural form. “Pending on each individual case history and clinical exam as well as family history of melanoma, we decide which moles need to be removed,” says Dr. Tsoukas.
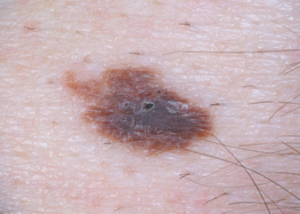
“We are focused on clinically appearing atypical nevi that under microscopic examination may have some abnormal features; however, do not meet all criteria to be identified as malignant melanoma.”
A patient may be concerned about one or two particular moles, perhaps due to size (they’re bigger than all the others on the patient’s body), or maybe they stand out because they’re darker than the rest.
For peace of mind, the patient then decides to have the moles electively removed. After all, the mindset might be, I know I can’t prevent melanoma from arising anywhere in my body, but at least I can prevent it from developing in these two particular moles.
Insurance won’t cover the cost of this if the only reason is peace of mind or anxiety.
Reimbursement logistics aside, Dr. Tsoukas says that in medicine, management and intervention are justified based on certain criteria and facts.
Otherwise, somebody would have medical care or intervention randomly decided.
Another reason that a person may have a mole electively removed is because of its location; it’s difficult for the individual to examine the mole as part of routine monthly skin exams.
But what if you have a lot of moles peppered all over your body?
It’s not practical to have every one of these spots systematically cut out or even “shaved” off.
On the other hand, what if many of these moles are on your back, which compounds the difficulty in keeping track of them for possible changes?
How do you draw a “mole map” of the spots on your back, unless you have an elaborate set-up with mirrors that frees up your hands (for sketching) and provides a clear view?
What if your ability to draw spots in a “map,” that accurately aligns with what you see in the mirror, is in sad shape?
And add to that this: Elective removal of many moles will cost a pretty penny and create a lot of hassle due to bandaging and removal of stitches.
If you have many skin lesions, including normal looking ones, it’s wise to get a yearly full-body skin exam.
A dermatologist will address moles that are clinically benign, those that show atypical features, and those that should be removed and biopsied.
“In addition,” says Dr. Tsoukas, “dermatologists use the mole mapping technique which combines photography, dermoscopy and a body map file created and saved electronically for each patient.”
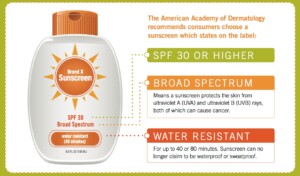
In addition to the skin exam, your dermatologist will explain additional risk factors for melanoma, which include skin type, family history of melanoma, sunburn history, age and even history of medications you’ve taken. You will also learn about sunscreen protection.

 clinical interests include diagnosis and management of patients at high risk for skin cancer, cutaneous oncology, laser surgery and aesthetic dermatology.
clinical interests include diagnosis and management of patients at high risk for skin cancer, cutaneous oncology, laser surgery and aesthetic dermatology.