An episode of atrial fibrillation may cause a mild elevation (“indeterminate range”) in troponin, but does this relate to a mortality or heart attack risk?
“In of itself, A-Fib does not cause a rise in troponin unless underlying coronary artery disease is also present,” says Dr. Adam Splaver, clinical cardiologist and co-founder of NanoHealth Associates, a practice that explores the molecular level of cardiovascular disease.
If atrial fibrillation is a suspected issue in a patient who presents in the ER with mildly elevated serial troponin results (that are falling), the next course of action would be to monitor the heart rhythm outside the hospital setting.
“Holter monitors, event recorders and loop recorders are just a few of the tools used to detect this arrhythmia, or disturbance in the heart’s normal rhythm,” says Dr. Splaver.
A-Fib is not treated with any kind of implanted device, but instead, with medications or ablation.
But it first has to be established that a patient even has A-Fib — and that’s done with the event monitors.
According to a report in the European Heart Journal, a mild elevation in troponin I in patients with atrial fibrillation is associated with increased risk of cardiac events and mortality. The report’s abstract states:
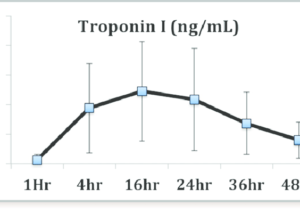
In patients with atrial fibrillation, minor troponin I elevation is regularly detected.
The study authors conclude that their findings may be important for risk stratification in such patients.
A report in Circulation has the same conclusion, except that the subjects also had an accompanying rapid ventricular rate:
Even mild troponin elevation in the setting of AFib with RVR predicts a significant increase in risk of MI at 1 yr. MI means a heart attack.
What would be very intriguing is a study of subjects, who’ve had CABG (coronary bypass surgery), who’ve had a mildly elevated troponin result as a consequence of atrial fibrillation.
Would the presence of bypass grafts impact the risk of future cardiac events and mortality?
Would it be slightly lower than patients in the same boat (severe heart disease) but who never had revascularization (bypass surgery)? Would the difference be negligible?