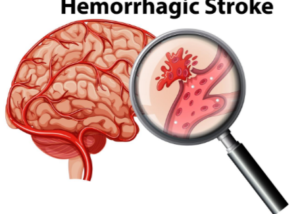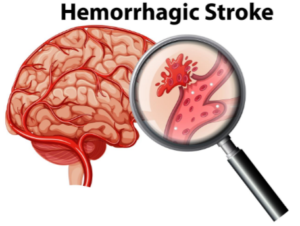
Often, a ruptured brain aneurysm means quick death, and if not, permanent brain damage. But these burst blood vessels do not always have to be lethal.
Surviving a Ruptured Brain Aneurysm
“The sooner the presence of an aneurysm is detected, the more likely it is to be successfully treated,” says Dr. Ezriel Kornel, Neurosurgeon, Principal with Brain & Spine Surgeons of New York, Medical Director of the Institute for Neurosciences at Northern Westchester Hospital, host of “Back Talk Live,” the weekly medical Web TV show.
“With a ‘full’ rupture, symptoms range from sudden death to coma to impaired level of consciousness, impaired speech and impaired motor function to simply an excruciating headache that does not let up,” continues Dr. Kornel.
What is the ruptured aneurysm (hemorrhagic stroke) headache like?
Dr. Kornel explains, “Always, it starts with a ‘thunderclap’ headache. About 50 percent of individuals with a full rupture of a cerebral aneurysm die before reaching a hospital, especially in more remote areas.
“A favorable outcome is certainly more likely if the aneurysm is discovered before there is a rupture that results in neurologic deficits.
“Over 60 percent of aneurysms are now treated by coiling, a procedure by which a very fine catheter is introduced into the aneurysm via arteries from the groin, into the head, and tiny ‘coils’ are injected into the aneurysm, filling it and causing it to clot off rather than bleed.
“Those aneurysms that cannot be coiled require clipping of the aneurysm microsurgically via a craniotomy.”
 Dr. Kornel is at the forefront of minimally invasive neurosurgery which he uses to treat brain tumors and other neurological ailments.
Dr. Kornel is at the forefront of minimally invasive neurosurgery which he uses to treat brain tumors and other neurological ailments.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.