Breast cancer can spread to the brain; why aren’t brain scans a standard part of lifelong surveillance?
Instead only the chest gets imaged at regular intervals.
For this question I spoke with Jonathan Stegall, MD, an integrative oncologist and medical director for The Center for Advanced Medicine, an adult cancer treatment center in Alpharetta, GA.
The lungs, liver and brain are the favored locations for breast cancer cells to spread to via the lymphatic system.
So are the bones. The bones are commonly the first location of metastasis.
I was inspired to investigate the peculiar phenomenon of chest-only imaging in patients with only bone mets after a relative of mine – who has BC bone mets – said that every three months, she undergoes only a chest scan.
Knowing that breast cancer can migrate to the brain, I asked, “Why don’t you also undergo head scans?”
She replied that it wasn’t necessary because a metastasis from bone mets would first go to the chest.
She added that it just wouldn’t be worthwhile to have that additional imaging.
I decided not to pursue the issue with her, but kept thinking about how she was playing Russian roulette, since it IS possible for breast cancer cells to migrate to the brain before to the lungs or liver.
Or isn’t it?
I dug deep with an online search and could not find anything in the medical literature confirming that BC cells in the bone – or even any dormant “hidden” ones in residual breast tissue following a double mastectomy – never ever make it to the brain before they travel to the chest!
Dr. Stegall says, “Breast cancer more commonly spreads to the chest before going to the brain.
“Triple negative and HER2 positive breast cancer spreads to the brain more often than hormone positive breast cancer does.”
My relative’s bone mets were finally discovered on an X-ray for upper arm pain that had been misdiagnosed as a musculoskeletal problem. (That’s a whole separate article – how this had gone over the heads of doctors who knew that she had a history of breast cancer!)
She underwent treatment with the drug Verzenio, which shrunk the masses.
The standard of care is for such patients to take a cancer fighting drug indefinitely and undergo lifelong imaging of the chest every three months.
Why don’t breast cancer patients with bone mets get ongoing brain scans?
“Brain imaging is typically reserved for cancer patients who exhibit symptoms concerning for brain metastases, such as chronic headaches, vision changes, speech changes, seizures, cognitive concerns, etc.,” says Dr. Stegall.
So this begs the question: Isn’t the prognosis better if a brain tumor is detected at one-millimeter via a surveillance scan rather than when it’s large enough to start causing symptoms?
What’s particularly vexing here is that BC brain mets can occur in multiples.
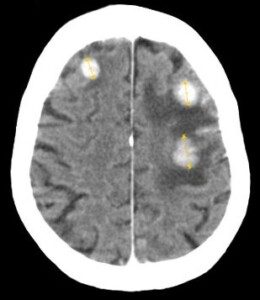
Breast cancer brain metastases. Jmarchn/creativecommons.org/licenses/by-sa/3.0/Wikimedia Commons
Dr. Stegall continues, “In an ideal world, proactive brain imaging for specific cancer types would be the standard, especially in patients who already have established metastases elsewhere or who have earlier stage cancers which have a preference for spreading to the brain.
“Unfortunately, this ultimately comes down to insurance coverage, which is typically not going to occur unless the patient is already having symptoms concerning for brain metastasis.”
This launches that million-dollar-question again: Why wait until a brain tumor is the size of a golf ball causing symptoms, when it can be much more easily treated if it’s tiny and asymptomatic?
“Brain metastases from breast cancer are an uncommon initial presentation of metastatic breast cancer,” says Dr. Stegall.
“It looks like about 10% of metastatic breast cancer patients initially present with brain metastasis.
“Brain imaging in breast cancer patients is typically reactionary in nature, if the patient develops concerning symptoms.
“In an ideal world, screening for this would be readily ordered and predictably reimbursed by insurance/Medicare/Medicaid.
“It does seem that there is more of a push to include this testing more regularly,” according to a study.
Here’s an excerpt from the paper:
“Brain-directed MRI screening for patients who harbor malignant neoplasms with potential for intracranial involvement is important given the impact of neurological compromise on quality of life.
“In addition, early identification of intracranial disease facilitates less invasive or less toxic approaches, such as stereotactic radiosurgery or careful use of promising systemic agents rather than WBRT or neurosurgical resection.”
Another point to consider is that some BC patients have enough money to easily pay for four brain scans a year.
Should they not be offered the option for brain imaging under the premise that it’s not impossible for the brain to be the first location for bone mets to migrate to?
Or, to put another way, there’s no procedure that can predict, with 100% accuracy, which patients will NOT be in that 10%!
“Cancer is so unpredictable, to the point that I think it is dangerous to assume that a patient who has not exhibited metastatic cancer in the chest couldn’t possibly have brain metastasis,” explains Dr. Stegall.
“While it’s not likely that a breast cancer patient develops more distant metastatic disease in the brain before developing it in the chest, it certainly occurs more often than we tend to think.
“Interestingly, the European Society for Medical Oncology (ESMO) recommends brain imaging such as brain MRI for breast cancer patients with metastatic HER2-positive or triple negative breast cancer (TNBC) who do NOT have symptoms, if the provider feels it might change their systemic therapy recommendations.
“This is based on the (very reasonable and logical) notion that brain metastases detected early can often be treated with interventions such as targeted radiation rather than more aggressive whole brain radiation, which is what we see with more advanced brain metastases.”
Russian Roulette
A patient might believe that the prognosis for secondary brain tumors that are discovered only after they start causing symptoms, is comparable to the prognosis of such a tumor if it were discovered on a surveillance brain MRI at only one-millimeter.
But waiting for the tumor to grow big enough to start causing symptoms might also mean that additional BC brain tumors have had a chance to pop up in different areas of the brain.
My relative has hormone positive BC. Last time I saw her I was impressed with her energy level.
At the time of this posting, her bone mets are stable; they have not progressed from their shrunken state.
But meanwhile, for all we know, there could be a secondary brain tumor brewing, that won’t be discovered until it begins causing the symptoms that will lead to a diagnostic brain MRI – which by then, there could be other smaller tumors throughout her brain.
How could her prognosis possibly be the same, when compared to if that hypothetical brain tumor were discovered during a screening MRI when it’s just a speck?
She’s playing Russian roulette. And yes, she has the money for at least two brain scans a year.
 Jonathan Stegall, MD, provides a long-awaited remedy for our cancer problem. Having a successful integrative oncology practice in Atlanta, GA, he’s seen firsthand what works and what doesn’t with cancer treatment. Dr. Stegall is the creator of the Cancer Secrets Podcast and author of “Cancer Secrets,” available on Amazon.
Jonathan Stegall, MD, provides a long-awaited remedy for our cancer problem. Having a successful integrative oncology practice in Atlanta, GA, he’s seen firsthand what works and what doesn’t with cancer treatment. Dr. Stegall is the creator of the Cancer Secrets Podcast and author of “Cancer Secrets,” available on Amazon.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.