If a tiny glioblastoma multiforme is spotted incidentally on a head CT for a different reason, could the patient be cured?
After all, average life expectancy following a GBM diagnosis is 14-16 months.
By the time a GBM is discovered via a head scan for symptoms suspicious for a brain tumor, the cancer is far from tiny.
A GBM is an incurable cancer, even though there are patients who survive several years after diagnosis.
“Although the average life expectancy after GBM diagnosis is 14-16 months, less than 1% of patients live 10 years,” says Jonathan Stegall, MD, an integrative oncologist and medical director for The Center for Advanced Medicine, an adult cancer treatment center in Alpharetta, GA.
“I have a patient who was diagnosed with GBM over six years ago and is doing great,” continues Dr. Stegall.
“He is my longest surviving GBM patient so far.”
Dr. Stegall notes the case of a woman, Carmen Rice, who as of 2023 has survived 17 years following her diagnosis of this merciless brain tumor.
Dr. Stegall also points out the case of a man, diagnosed at 47, who survived 20 years (as of 2021) without any tumor recurrence.
The study authors point out that “…the exact contribution for extended survival is still not known,” referring to not just this 20-year-case, but also cases in which people have lived 10+ years out from GBM diagnosis.
Does a very small GBM mean a longer survival time, let alone cure?
The study says that a better prognosis has been found to be associated with “patients’ characteristics,” plus “biological factors that impact tumor aggressiveness [tumor genetics], and/or factors associated with treatment.”
The paper points out that a younger age at diagnosis is “the most important factor for long survival,” and that most of these reported cases are in patients under 40.
There is no mention of small size or early detection of a GBM being predictive of longer survival.
As mentioned, glioblastoma multiforme is considered an incurable cancer.
Thus, the concept of some cases actually being cured does not exist.
“I can’t find anyone who has lived 30 years,” says Dr. Stegall.
In summary, there is no data on the correlation between small GBM’s or early diagnosis with a longer survival.
There is also no research on survival rates of glioblastoma multiformes that were discovered incidentally, when too small to cause symptoms.
An example of an incidental discovery of a GBM would be during a brain scan for head trauma sustained in a car accident.
Average Size of a GBM at Diagnosis
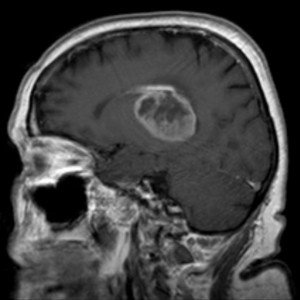
GBM. Credit: Hellerhoff
A report says it’s 4 cm, according to one study. Another study, says this paper, names an average size of five to 10 cm, while a very small percentage of cases involved a tumor over 10 cm.
Another report gives details on the genetics of a GBM impacting survival time.
It would seem, based on logic, that if a GBM of just 2 mm (the size of a small mole) were discovered by accident during an MRI for a suspected brain bleed from trauma, that this mole-sized tumor could be more easily eradicated via surgery, radiation and chemotherapy.
However, just because the GBM was so tiny doesn’t mean it can’t come back a few years later, resulting in death within a few years.
Related is a study of incidentally discovered GBM’s and survival time, but just because the tumor in these four patients was discovered during a head scan for an unrelated reason doesn’t mean that the masses were exceptionally small.
The study looked at only a comparison between incidentally discovered and diagnostically discovered tumors.
Survival of these patients was only marginally longer than survival in the 234 other patients whose tumors were confirmed after undergoing imaging for symptoms.
Summary
• Research is lacking in the correlation between length of survival after a GBM diagnosis and either how small it was at diagnosis or how early in growth it was.
• This brain tumor is deemed as incurable.
• Long-term survival is very uncommon, and reasons for such still remain in the theoretical realm.
• It’s not surprising, though, that younger age at diagnosis would be the strongest association for longer survival rates, since younger bodies generally respond better than do older bodies to aggressive cancer treatments.
Breakthrough May Extend Life for GBM Patients
A promising investigation led by Keck Medicine of USC discovered that a trio of therapies, when used together, may considerably increase the survival time of patients.
This approach combines tumor treating fields (TTFields) — a wearable device that emits gentle electrical fields targeting cancer cells — with standard chemotherapy and the immunotherapy drug pembrolizumab.
TTFields generate low-intensity, alternating electrical fields that interfere with how cancer cells multiply.
These fields are delivered through soft adhesive patches on the scalp that patients wear 18 hours daily.
The technology is designed to impact only the tumor, leaving healthy brain tissue unaffected.
By itself, this treatment slows or halts growth of cancer cells.
However, this study revealed that TTFields also encourage an immune reaction by attracting T cells into the tumor’s surroundings.
Once these T cells are inside the tumor, pembrolizumab further enhances their cancer fighting activity.
What the Study Found
The triple therapy approach led to a 70% increase in patient survival compared to those who previously received only TTFields and chemotherapy.
The therapy was particularly effective in patients with large, non-operable tumors.
Larger tumors may present more recognizable targets for both the immune system and the electric field therapy.
Surgical removal may reduce the immune system’s ability to recognize the tumor.
How was this study done?
The team launched a clinical trial including 31 people recently diagnosed with GBM.
All participants had already undergone radiation therapy.
Out of the 31, 26 received the complete treatment regimen: TTFields, chemotherapy and pembrolizumab.
Among them, seven had tumors that could not be surgically removed due to their location.
Patients continued this combined treatment for up to 24 months.
On average, those receiving all three therapies lived approximately 10 months longer than previous patients who had only received TTFields and chemotherapy.
Inoperable tumor patients saw an even greater benefit, living around 13 months longer.
As of mid-2025, Keck Medicine is taking part in a broader, Phase 3 clinical trial to further validate these findings.
This expanded trial aims to enroll over 740 patients and is currently underway across research sites in the United States, Europe and Israel.
 Jonathan Stegall, MD, provides a long-awaited remedy for our cancer problem. Having a successful integrative oncology practice in Atlanta, GA, he’s seen firsthand what works and what doesn’t with cancer treatment. Dr. Stegall is the creator of the Cancer Secrets Podcast and author of “Cancer Secrets,” available on Amazon.
Jonathan Stegall, MD, provides a long-awaited remedy for our cancer problem. Having a successful integrative oncology practice in Atlanta, GA, he’s seen firsthand what works and what doesn’t with cancer treatment. Dr. Stegall is the creator of the Cancer Secrets Podcast and author of “Cancer Secrets,” available on Amazon.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.



































