Many pulmonary embolisms in hospital settings cause sudden death without symptoms, but many people die even when there are warning signs.
You may be thinking that it takes about four minutes for irreversible brain damage to occur when a patient has been deprived of oxygen (airflow blocked by a massive pulmonary embolism).
You may then be thinking that between symptom onset and death, medical personnel have four minutes to re-establish airflow.
However, people in hospitals have died from a pulmonary embolus even when there was more “brain time” involved.
In that case, the patient was still conscious and breathing (albeit very labored) after initial PE symptom onset.
“Massive PEs or saddle embolisms have a high risk for being fatal in any setting,” says Paul Lucas, MD, a surgeon with the Vascular Center and director of the Vascular Laboratory at Mercy Hospital in Baltimore.
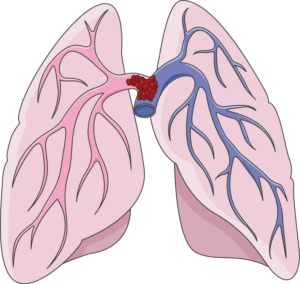
A “saddle” pulmonary embolism, plugging up the point at which the pulmonary artery branches off into each lung. Death can occur suddenly. Laboratoires Servier, CC BY-SA 3.0 /creativecommons.org/Wikimedia Commons
“Events occurring in a hospital, or at any site for that matter, require a trigger of a sequence of events to occur …. time of event to intervention,” continues Dr. Lucas.
“Although we would all like this to be instantaneous, it does take time. Every effort is made in these emergencies to expedite this.”
Treatment of Pulmonary Embolus Has Risks
“Keep in mind, you have to have a strong suspicion/diagnosis for this entity to just administer “clot busters,” as other things can have similar presenting symptoms,” says Dr. Lucas.
“You certainly don’t want to give ‘clot busters’ to someone whose symptoms are from that of bleeding.”
Here is what Steven Elias, MD, a vein specialist with Englewood Health in NJ, says:
“Before starting any therapy [i.e., blood thinners) that has significant risk such as intracranial bleeding (bleeding in the brain), most MDs would like a definitive diagnosis.
“If a patient survives a ‘massive PE’ and doesn’t immediately die, there is usually time for a CT scan which takes about 1-2 minutes.”
 Dr. Lucas leads a team of vascular surgeons and technologists who specialize in the diagnosis and treatment of patients with diseased blood vessels.
Dr. Lucas leads a team of vascular surgeons and technologists who specialize in the diagnosis and treatment of patients with diseased blood vessels.
 Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
Dr. Elias is a leading name in venous disease, minimally invasive vein disease therapy and clinical vein and wound research. Dr. Elias lectures about all aspects of venous disease nationally and internationally.
 Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
Lorra Garrick has been covering medical, fitness and cybersecurity topics for many years, having written thousands of articles for print magazines and websites, including as a ghostwriter. She’s also a former ACE-certified personal trainer.
.