
Being that sleep apnea causes frequent low oxygen levels overnight, could a finger pulse oximeter by itself detect sleep apnea?
When sleep apnea is suspected, the patient is encouraged to undergo a “sleep study” (polysomnography) at a lab — and if that’s absolutely not possible, one can take a sleep study test at home overnight.
There have been a few studies showing, to a degree, some effectiveness of the pulse oximeter at indicating the presence of OSA.
This is contingent on the device recording abnormally low levels of oxygen in the blood, called desaturation, which results when the patient has paused episodes of breathing.
However, “Not all apnea produces desaturation,” says Dr. Nancy Foldvary-Schaefer, DO, MS, and Director, Sleep Disorders Center, Cleveland Clinic.
“Oximetry only picks up 3-4% desats depending on the threshold of the device. That is a significant drop in saturation especially in patients with normal lung function.
“In patients with normal lung function, it takes a longer apnea or hypopnea to produce an oxygen desaturation.
“Sometimes the desaturation is only 1-2%, which is very minor and would not be identified on an oximetry test.
“Some obstructive events produce an arousal without a desaturation, which is why home sleep testing underestimates OSA severity (no EEG electrodes, so sleep is not recorded).”
UARS can cause an arousal without a desaturation. This stands for upper airway resistance syndrome — created by a partially blocked, rather than completely blocked, upper airway.
The daytime symptoms may mimic obstructive sleep apnea even though overnight oxygen levels remain normal.
This is because apneas do not occur, but labored breathing does.
Because of the patient’s airway defect, the brain is repeatedly aroused just enough to induce a high respiratory workload (“heavy breathing” but not snoring).
These repeated arousals prevent the brain from achieving adequate restoration – which can cause daytime symptoms like sleepiness.
And the pulse oximeter would never show abnormally low oxygen levels.
A Study Shows what a Pulse Oximeter Can Do
According to a comprehensive analysis (Netzer et al, Chest, August 2001) of medical literature about pulse oximetry and sleep disordered breathing, the little device can be a “very useful tool for the diagnosis of sleep-disordered breathing.”
Oximetry data is always part of the sleep studies at labs or home polysomnography.
The study says that the pulse oximeter can be a screening tool for OSA.
However…
The paper also points out that pulse oximetry has limitations — stemming from issues with blood flow or a lack of change in oxygen saturation.
Because pulse oximetry relies upon pulsatile flow of blood for its data, it’s vulnerable to the effects of poor peripheral (extremities) arterial blood flow.
What this means is that during sleep, the patient’s natural and apnea-triggered body movements, plus blood vessel constriction and low blood pressure during apneas, can throw off the measurements.
The body movements cause what are known as artifacts. The oximeter device doesn’t always detect these, leading to overestimation of inadequate oxygen (desaturation).
Obesity may further trip up the accuracy of oxygen measurements due to “tissue optics.”
Another point to consider: An overnight drop in oxygen levels can be caused by chronic heart failure — which can also coexist with obstructive sleep apnea.
A person with CHF may have desaturation, but this doesn’t automatically mean they have an obstructed airway during sleep.
If you suspect sleep apnea but recently had a negative overnight pulse oximeter result, you should consider a sleep study – preferably at a lab.
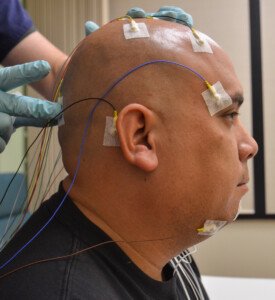
Preparing for a lab sleep study.
Even if you’ve read about a study showing an OSA detection rate of 90% accuracy with the pulse oximeter, this is nowhere as accurate as a lab polysomnography.
Though a polysomnography can produce a false-negative very uncommonly, a repeat polysomnography in such a case, with someone who has clinical features of OSA, is certainly far more sensitive and specific to detection than is a pulse oximetry.
Furthermore, a sleep study will show the grade of OSA: mild, moderate or severe. A pulse oximeter won’t.
This data helps in the calibration of CPAP treatment.

 Certified by the American Board of Neurology and Psychiatry in Neurology, Clinical Neurophysiology and Sleep Medicine,
Certified by the American Board of Neurology and Psychiatry in Neurology, Clinical Neurophysiology and Sleep Medicine, 









