
Be on the lookout for specific things that should be done in the ER when an elderly woman complains of chest pain.
If an elderly family member is having chest pain, don’t delay getting them to the emergency room.
I’ve taken my elderly mother to the ER for chest pain multiple times. So I know exactly what happens in the ER when an elderly individual reports chest pain.
• Intake where basic questions are asked about medical history.
• Wheeled to a room.
• Set up to devices that record heart rate, blood pressure and pulse, and oximeter on the fingertip to measure body oxygen level.
• Supplemental oxygen through the nose (“The heart likes oxygen,” one nurse said). However, at least one ER visit didn’t have this done.
• Nurse sets up a port in the patient’s arm through which blood samples can be drawn and drugs administered.
• Nurse will ask basic questions such as nature of the chest pain.
If the only complaint by an elderly person is chest pain, yet the patient can still talk and is not struggling to breathe, there will be some waiting for a doctor, though not long.
This will vary depending on how many more urgent cases (e.g., an elderly patient vomiting pink froth along with chest pain) there are.
The doctor will ask for a medical history such as previous surgeries, current medications, smoking status, etc., and will also ask for a description of the chest pain.
The doctor will also ask details such as, “Is the pain triggered only with exertion,” or, “Does it hurt when I lift your arms like this?”
The doctor will conduct other tests such as examining the patient’s ankles (for signs of congestive heart failure), pressing (palpating) the abdomen and listening to the chest and back through a stethoscope.
Four Main Tests Ordered on Every ER Visit for Chest Pain
• Chest X-ray
• EKG – 12 leads
• Troponin
• D-Dimer
I was reading another “what to expect in the ER for chest pain” article on another popular site, and it excluded the D-dimer. This is unacceptable.
A report of chest pain should always net a D-dimer test! More on that coming up.
But first, the chest X-ray is always taken despite the cumulative radiation exposure. More on that shortly.
The troponin blood test is a must. Troponins are enzymatic proteins that are released into the bloodstream by cardiac tissue when heart muscle is damaged from a heart attack.
The initial result, available within 30 minutes, may be normal. If the result is normal, it is NOT time to leave.
When a heart attack occurs, it can take several hours for troponins to elevate enough in the bloodstream to show positive on the test.
This is why a second test will be ordered. In fact, if the first result is abnormal, a second test is still ordered. Serial testing will show a trend.
Sometimes a third test (several hours after the second) is ordered.
This is why a complaint of chest pain means a lengthy ER stay. Depending on the doctor, there can be six hours between troponin blood draws.
What to Expect if D-Dimer Is Positive
The D-dimer test checks the body for the presence of a blood clot. If this test is positive, this suggests (not guarantees) a blood clot somewhere.
A blood clot in a lung, called a pulmonary embolus, can cause chest pain — not to mention sudden death.
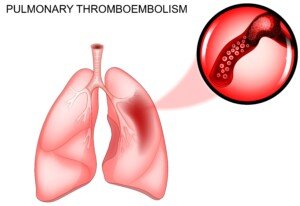
Shutterstock/Artemida-psy
• Doctor will recommend a CT scan of the lungs if the D-dimer is positive.
• The older the patient, once in the elderly range, the less significant a positive D-dimer is. Just being very old can yield a positive result.
• Every single time, my mother’s D-dimer was positive. And every single time the CT scan was ordered. Doctors cannot take any chances, even though they know that elderly status often results in a false-positive D-dimer.
Why the Chest X-ray?
• Chest pain can be caused by pneumonia, which the X-ray will show.
• This common symptom can also be caused by an aortic aneurysm, visible on the X-ray.
Now for example, if there was no aortic aneurysm detected on an X-ray three months ago, it’s not considered that suddenly, the patient has a large aneurysm causing chest pain 90 days later.
However, pneumonia can occur suddenly in the elderly at any time, and this is reason enough for that X-ray to be taken no matter how many ER visits in a short time span.
Abnormal EKG
• Though an EKG can sometimes indicate coronary artery blockage, sometimes it won’t.
• My mother’s EKG always shows a “bundle branch block.”
• Other than the bundle branch block, my mother’s EKG showed no indication of the severely blocked arteries that caused her first bout with chest pain.
What Else?
Not much. Most of the time will be spent doing nothing while waiting on the second (or third) troponin test.
If these are normal, and all other tests are normal, the patient is discharged — with instructions to follow up with their primary physician.
Warning to Caregivers
An elderly patient may think it’s time to go home when that first troponin test comes back normal.
The family member or friend who is with them must urge them to stick around for that second blood draw.
Don’t be surprised if you get resistance, but stick to your guns. My mother’s second blood draw, on her second-ever ER visit for chest pain, yielded a “grey range” result.
This wasn’t in the definite heart attack range, but it wasn’t in the normal range, either. The doctor wanted her admitted.
She resisted this and I fought back and talked her into it. Two days later she underwent a quintuple bypass surgery and heart valve replacement!
All of my elderly mother’s subsequent complaints of chest pain turned out to be nothing, but a history of “nothing” by no means should alter standard of medical care in the emergency room.











